Prostate cancer | Cáncer de próstata ✨
Greetings, friends of Hive
We continue to join this call, bearing in mind that "cancer" is a generic term that includes nosological entities (diseases), which have as a similar characteristic, the accelerated and uncontrolled multiplication of cells that invade and colonize tissues, organs, apparatus and systems, where it can occur in any part of the body.
In men, in general, the most frequent types of cancer are prostate cancer, lung cancer, colorectal cancer and bladder cancer. On this occasion, we will refer to prostate cancer.
We will begin this tour with basic aspects of anatomy (body structure). We will try to condense the information as much as possible, but it is important to familiarize yourself with it.
Male urogenital anatomy
The name urogenital is used because the urinary and reproductive systems in men merge and overlap anatomically, by using a common organ, which is the urethra.
Structurally, the male urogenital system is made up of the scrotum, testicles, epididymis, vas deferens, seminal vesicles, ejaculatory ducts, bulbourethral glands, urethra, penis and prostate.
Each organ listed above fulfills a specific task and together, they work in harmony and synchrony for a vital function, which is to contribute to human reproduction, through the production, storage and transport of spermatozoa.
 Diagram of the male internal urogenital anatomy. Lateral view.
Diagram of the male internal urogenital anatomy. Lateral view.Credits: Alt.sex and Tsaitgaist . Used under CC 3.0 license.
Below is a description of each structure (see diagram):
Scrotum: these are two skin sacs that surround and protect the testicles. They control the temperature in that area, so that it is lower than the body temperature.
Testes: two glands that produce gametes (sperm) and the sex hormone (tetosterone).
Epididymis: two spiral ducts located above each testicle. They store the spermatozoa so that they can mature and become motile.
Vas deferens: two ducts that facilitate the transport of sperm from the epididymis to the seminal vesicles.
Seminal vesicles: there are two seminal vesicles, which produce substances to nourish the sperm.
Ejaculatory ducts: these are two small ducts. They collect fluids and substances to form seminal fluid (semen). These ducts also carry semen from the testicles to the urethra.
Bulbourethral glands: two glands that produce a secretion (preseminal fluid) that lubricates the head of the penis during erection and ejaculation.
Urethra: passageway for urine during urination, preseminal fluid during erection and seminal fluid during ejaculation.
Penis: copulatory and urinary organ. It allows the passage of urine, preseminal fluid and seminal fluid.
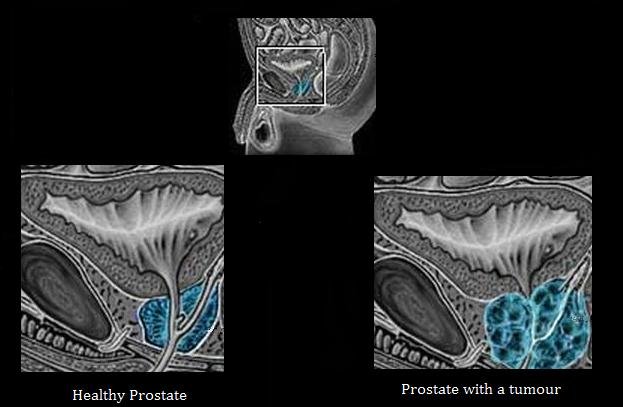
The prostate
It is a gland located below the bladder (organ that stores urine), in front of the rectum (final part of the intestine) and surrounds the urethra.
It produces a fluid (prostatic antigen) that protects the sperm and promotes their mobility.
It functions as a valve during sexual intercourse, stopping the passage of urine and allowing the passage of pre-seminal fluid and semen.
It protects against germs and bacteria from the outside, favoring the infrequency of urinary tract infections in men.
It tends to grow as men age.
What is prostate cancer?
Prostate cancer is when the cells of this gland are altered in their growth and development, multiplying uncontrollably (malignant) and form tumors.
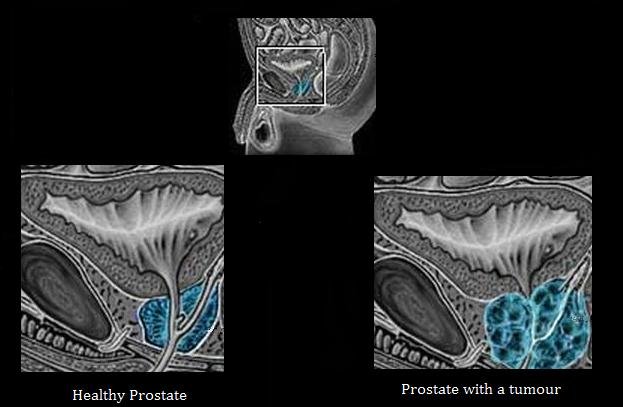 Differences between healthy prostate and a prostate with a tumour
Differences between healthy prostate and a prostate with a tumourCredit: BQmUB2012102. Used under CC 3.0 license.
Some variants of prostate cancer grow slowly and may require minimal treatment, while other types are considerably aggressive and can spread very rapidly.
The occurrence and development of prostate cancer in men under 40 years of age is rare, but after the age of 50, the probability increases rapidly.
Signs and symptoms
It is a type of cancer, with variable symptomatology and without a specific pattern to refer. Sometimes it is asymptomatic (no signs or symptoms) in patients, in others the signs and symptoms that occur are variable.
The signs and symptoms described are related and associated with urinary tract obstruction:
- Pain or burning to urinate.
- Need to urinate more often than usual, during the day and night, or predominantly at night.
- Involuntary loss of urine.
- Weak or interrupted urine flow (urine stream); with the need to strain to empty the bladder.
- Blood in the urine or semen.
- Inability to urinate.

- Post-urination dribbling.
- Pain on ejaculation.
- Onset of erectile dysfunction (difficulty maintaining an erection).
- Feeling of heaviness in the rectum or change in bowel habits.
- Persistent pain in the back, hips or pelvis.
- Weight loss for no apparent reason.
- Fatigue.
Keep in mind that the symptomatology described above may occur in diseases other than prostate cancer. For example, Benign Prostatic Hyperplasia (enlargement of the prostate associated with age) can produce similar symptoms as well as a bladder or kidney infection.
Diagnosis
The ideal diagnosis is to detect prostate cancer before it generates symptomatology (signs and symptoms), that is, to find it early (incipient), before it spreads, and to initiate treatment in a timely manner.
Although there is no standard test to detect prostate cancer, this slow-growing tumor has methods for its early detection and they are:
- Prostate Specific Antigen (PSA) test:
It is a blood test, which measures the level of Prostate Specific Antigen (PSA). This substance is produced by the prostate and its levels are usually elevated in patients with prostate cancer. However, other factors and other conditions can increase PSA levels.

- Digital rectal examination (DRE), the prostate is palpated through the rectal wall looking for nodules, irregularities, increased consistency, alterations in the borders or abnormal areas of the gland.
These studies must be linked to an adequate physical examination and clinical history that includes personal and family history, pathological antecedents, habits, lifestyles, among other aspects.
The treating physician will be the patient's expeditious guide and together they will conciliate through the pertinent informed consents, the need and approval of these and other studies such as biopsy (small sample of prostate tissue) or imaging (ultrasound, magnetic resonance), etc.
Treatment
There are several types of behaviors to follow for the treatment of prostate cancer. It will be the patient together with his treating physician, considering the affectation, who will decide the course to follow. Some of the treatments that are carried out:
- Active surveillance: medical control and periodical prostatic antigen.
- External radiotherapy: radiation to the cancerous cells by means of a machine external to the body.
- Brachytherapy: through surgery, radioactive seeds or pills are introduced into or near the tumor to destroy the malignant cells.

- Surgery: operation to remove the prostate (prostatectomy) and the surrounding tissue.
- Radiotherapy plus hormone therapy.
- Chemotherapy: administration of special drugs to reduce the size of the cancerous tumor or eliminate it.
Can prostate cancer be prevented?
To date, there are no scientifically proven protective factors that guarantee the prevention of prostate cancer.
But it is possible to adopt healthy measures that protect your health in a comprehensive manner, such as :
- Balanced diet, with consumption of vegetables, fruits and whole grains; avoiding foods high in fat and refined sugars.
- Drinking between two and three liters of water a day.
- Develop physical activity, according to age.
- Avoid smoking and reduce alcohol consumption.
- Every man over 40 should have an annual medical evaluation specialized in the urogenital sphere and undergo PSA and DRE; especially those with a family history of prostate cancer.
In tune, practice self-care, pay attention to the signals your body gives off, such as warning messages through signs and symptoms.
Go regularly to your health controls, with specialized assessment and periodic diagnostic tests, only in this way there will be an early detection of cancer.
 Credit: Tyler Nix. Public domain.
Credit: Tyler Nix. Public domain.
Español
Saludos, amigos de Hive
Seguimos sumándonos a esta convocatoria, teniendo en cuenta que "cáncer" es un término genérico que incluye entidades nosológicas (enfermedades), que tienen como característica similar, la multiplicación acelerada e incontrolada de células que invaden y colonizan tejidos, órganos, aparatos y sistemas, donde puede presentarse en cualquier parte del cuerpo.
En los hombres en general, los tipos de cáncer más frecuentes son el de próstata, el de pulmón, el colorrectal y el de vejiga. En esta ocasión, nos referiremos al cáncer de próstata.
Comenzaremos este recorrido con aspectos básicos de anatomía (estructura corporal). Intentaremos condensar la información al máximo, pero es importante que se familiarice con ella.
Anatomía urogenital masculina
La denominación urogenital se utiliza, porque los sistemas urinario y reproductivo del hombre, se fusionan y se superponen anatómicamente, mediante un órgano común, que es la uretra.
Estructuralmente el aparato urogenital masculino, está formado por el escroto, los testículos, el epidídimo, los conductos deferentes, las vesículas seminales, los conductos eyaculadores, las glándulas bulbouretrales, la uretra, el pene y la próstata.
Cada órgano mencionado cumple una tarea específica y juntos, trabajan en armonía y sincronía para una función vital, que es contribuir a la reproducción humana, mediante la producción, el almacenamiento y el transporte de espermatozoides.

Diagrama de la anatomía interna urogenital masculina. Vista lateral.
Créditos: Alt.sex,Tsaitgaist y Angelito7 . Usado bajo licencia CC 3.0.
A continuación encontrará una descripción de cada estructura (consulte el diagrama):
Escroto: son dos sacos de piel que rodean y protegen los testículos. Controlan la temperatura en esa zona, para sea inferior a la corporal.
Testículos: dos glándulas que producen gametos (espermatozoides) y la hormona sexual (tetosterona).
Epidídimo: dos conductos en espiral, situados encima de cada testículo. Almacenan los espermatozoides, para que maduren y adquieran movilidad.
Conductos deferentes: dos canales que facilitan el transporte de los espermatozoides, desde el epidídimo hasta las vesículas seminales.
Vesículas seminales: existen dos y producen sustancias para nutrir los espermatozoides.
Conductos eyaculadores: son dos pequeños conductos. En ellos se juntan fluídos y sustancias, para formar el líquido seminal (semen). Así mismo, estos conductos transportan el semen, de los testículos a la uretra.
Glándulas bulbouretrales: dos glándulas que producen una secreción (líquido preseminal) que lubrica la cabeza del pene, durante la erección y la eyaculación.
Uretra: conducto que permite el paso de la orina durante la micción, del líquido preseminal durante la erección y el líquido seminal durante la eyaculación.
Pene: órgano copulador y urinario. Permite el paso de la orina, del liquido preseminal y seminal.
La próstata
Es una glándula situada debajo de la vejiga (órgano que almacena la orina), delante del recto (parte final del intestino) y rodea a la uretra.
Produce un líquido (antígeno prostático) que protege los espermatozoides y favorece su movilidad.
Funciona como una válvula durante el acto sexual, deteniendo el paso de la orina y permitiendo el paso del líquido preseminal y seminal.
Protege contra los gérmenes y bacterias del exterior, favoreciendo la poca frecuencia de infecciones urinarias en los hombres.
Tiende a crecer a medida que los hombres envejecen.
¿Qué es el cáncer de próstata?
El cáncer de próstata se produce cuando las células de esta glándula sufren alteraciones en su crecimiento y desarrollo, multiplicándose de forma incontrolada (maligna) y formando tumores.
Diferencias entre próstata sana y próstata con tumor.
Crédito: BQmUB2012102 . Usado bajo licencia CC 3.0.
Algunas variantes del cáncer de próstata crecen lentamente y pueden requerir un tratamiento mínimo, mientras que otros tipos son considerablemente agresivos y pueden extenderse muy rápidamente.
La aparición y el desarrollo del cáncer de próstata en hombres menores de 40 años es poco frecuente, pero a partir de los 50 años la probabilidad aumenta rápidamente.
Signos y síntomas
Es un tipo de cáncer, con sintomatología variable y sin un patrón específico que referir. En ocasiones es asintomático (sin signos ni síntomas) en los pacientes, en otras los signos y síntomas que se presentan son variables.
Los signos y síntomas, descritos están relacionados y asociados con la obstrucción de las vías urinarias:
- Dolor o ardor al orinar.
- Necesidad de orinar con más frecuencia de lo habitual, durante el día y la noche, o a predominantemente por la noche.
- Pérdida involuntaria de orina.
- Flujo de orina débil o interrumpido (chorro de orina) ; con necesidad esforzarse para vaciar la vejiga.
- Sangre en la orina o el semen.
- Incapacidad para orinar.

- Goteo después de orinar.
- Dolor a la eyaculación.
- Aparición de disfunción eréctil (dificultad para mantener la erección).
- Sensación de pesadez en el recto o cambio en los hábitos intestinales.
- Dolor persistente en la espalda, las caderas o la pelvis.
- Pérdida de peso sin motivo aparente.
- Fatiga.
Tenga presente que la sintomatología descrita anteriormente, puede darse en enfermedades distintas al cáncer de próstata. Por ejemplo, la Hiperplasia Prostática Benigna (agrandamiento de la próstata asociado a la edad) puede producir síntomas similares, así como una infección de vejiga o riñón.
Diagnóstico
El diagnóstico ideal es detectar el cáncer de próstata antes de que genere sintomatología (signos y síntomas), es decir hallarlo temprano (incipiente), antes de que se disemine, e iniciar el tratamiento oportunamente.
Aunque no existe una prueba estándar para detectar el cáncer de próstata, este tumor de crecimiento lento, cuenta con métodos para su detección temprana y son:
- Prueba del Antígeno Prostático Específico (PSA, por sus siglas en inglés) :
Es un análisis de sangre, que mide el nivel del Antígeno Prostático Específico (PSA). Esta sustancia es producida por la próstata y sus niveles suelen ser elevados en pacientes con cáncer de próstata. No obstante, otros factores y otras afecciones pueden aumentar los niveles de PSA.

- Tacto rectal (DRE siglas en inglés), se palpa la próstata a través de la pared rectal en busca de nódulos, irregularidades, aumentos de consistencia, alteraciones en los bordes o zonas anormales, de la glándula.
Estos estudios deben estar ligados a un adecuado exámen físico e historia clínica que incluya antecedentes personales, antecedentes familiares, antecedentes patológicos, hábitos, estilos de vida, entre otros aspectos.
El médico tratante será el guía expedito del paciente y juntos conciliarán a través de los consentimientos informados pertinentes, la necesidad y aprobación de estos y otros estudios como biopsia (pequeña muestra de tejido prostático) o imagenología (ecografías, resonancia magnética), etc.
Tratamiento
Existen varios tipos de conductas a seguir para el tratamiento del cáncer de próstata. Será el paciente junto con su médico tratante, considerando la afectación, quienes decidan el curso a seguir. Algunos de los tratamientos que se llevan a cabo:
- Vigilancia activa: control médico y antígeno prostático
periódico. - Radioterapia externa: radiación a las células cancerosas mediante una máquina externa al cuerpo.
- Braquiterapia: mediante cirugía, se introducen semillas o píldoras radiactivas en el tumor o cerca de él para destruir las células malignas.

- Cirugía: operación para extirpar la próstata (prostatectomía) y el tejido circundante.
- Radioterapia más terapia hormonal.
- Quimioterapia: administración de fármacos especiales para reducir el tamaño del tumor canceroso o eliminarlo.
¿Se puede prevenir el cáncer de próstata?
Hasta la fecha, no existen factores de protección científicamente probados, que garanticen la prevención del cáncer de próstata.
Pero si es posible adoptar medidas saludables que protejan su salud de forma integral, como :
- Dieta equilibrada, con consumo de verduras, frutas y cereales integrales; evitando alimentos ricos en grasas y azúcares refinados.
- Beber entre dos y tres litros de agua al día.
- Desarrollar actividad física, de acuerdo con la edad.
- Evitar fumar y reducir el consumo de alcohol.
- Todo hombre mayor de 40 años debe realizarse una evaluación médica anual especializada en la esfera urogenital y someterse a PSA y DRE; especialmente aquellos con antecedentes familiares de cáncer de próstata.
En sintonía, practique el autocuidado, preste atención a las señales que emite su cuerpo, como mensajes de alerta a través de signos y síntomas.
Acuda regularmente a sus controles de salud, con valoración especializada y pruebas diagnósticas periódicas, solo así habrá una detección precoz del cáncer.
 Crédito: Tyler Nix. Dominio público.
Crédito: Tyler Nix. Dominio público.Bibliographic references consulted / Referencias bibliográficas consultadas
-American Cancer Society. Prostate cancer. [Internet]. 2020. [quoted 2023 Feb.] Available at
-American Society of Clinical Oncology (ASCO). Prostate cancer [Internet]. 2023 [quoted 2023 Feb.] Available at
-Centers for Disease Control and Prevention (CDC). Prostate cancer. [Internet]. 2022. [quoted 2023 Feb.] Available at
-Healthengine. Male reproductive system (urogenital system) anatomy [Internet] 2006 [quoted 2023 Feb]. Available at
-National Cancer Institute (NIH). Prostate cancer. [Internet] [quoted 2023 Feb]. Available at
-Sociedad Española de Oncología Médica (SEOM). Cáncer de próstata. [Internet]. 2021. [quoted 2023 Feb.] 89(9):731-738. Available at
PD: This article has been designed in ecency front-end. Variations may occur if viewed on another front-end.
PD: Este artículo ha sido diseñado en front-end ecency. Pueden producirse variaciones si se visualiza en otro front-end.

Sobre mí Soy venezolana. PhD. Médico Parasitólogo-Protozoólogo. Formada en Salud Colectiva, Ciencias Médicas Fundamentales, Filosofía de la Ciencia y Gestión Educativa.
Sobre la portada: es una producción original realizada con el programa Canva (versión gratuita), utilizando elementos libres de regalías. El avatar es producto de una fotografía de mi propiedad, procesada con la aplicación Toonlab. En la portada se incluyó una imagen esta es la fuente.La producción escrita ha sido creada esclusivamente para esta participación.
https://twitter.com/1519360679899275265/status/1630425763676602368
https://twitter.com/134311926/status/1631241204342960128
The rewards earned on this comment will go directly to the people( @marilour, @alummno ) sharing the post on Twitter as long as they are registered with @poshtoken. Sign up at https://hiveposh.com.
Yay! 🤗
Your content has been boosted with Ecency Points, by @almajandra.
Use Ecency daily to boost your growth on platform!
Support Ecency
Vote for new Proposal
Delegate HP and earn more
Greetings @almajandra, very grateful for your support. Thank you @ecency team I appreciate it.
You're welcome @marilour. Thanks @ecency for the support.
all forms of cancer are bad. thank you for informing us about this.
Hello @ipexito nice to greet you, thank you for visiting and reading. Yes you are right; but we have to raise awareness about it. Keep in mind that it can be cured if we detect it in time. Also encourage healthy lifestyles.
Until another time.
Happy and blessed week.
Long time away from life science. Thanks for the discussion.
Hi, @th4488 good to see you around, thanks for giving the post a read. The Med-Hive community is the hive health community. It promotes, encourages health and healthy lifestyles. Whenever you like you can join and if you wish you can participate in their initiatives.
See you another time.
Happy and blessed week.
Excelente publicación, @marilour! Muchas gracias por recordarnos de este importante tema. Dios te bendiga!
!LUV
!POB
!DIY
Saludos @acgalarza agradecida por sus bendiciones y amables palabras. Lo hago con gusto, Hive es un espacio con muchas bondades para fomentar y promocionar la salud. El cáncer es curable si lo diagnosticamos a tiempo.
Feliz y bendecida semana
Muchas gracias por los regalos
!LUV
@acgalarza, @marilour(2/3) sent you LUV. | tools | discord | community | HiveWiki |
HiveWiki |  NFT | <>< daily
NFT | <>< daily
Totalmente de acuerdo
Igualmente 🤗
!PGM
!PIZZA
!PAL
BUY AND STAKE THE PGM TO SEND A LOT OF TOKENS!
The tokens that the command sends are: 0.1 PGM-0.1 LVL-0.1 THGAMING-0.05 DEC-15 SBT-1 STARBITS-[0.00000001 BTC (SWAP.BTC) only if you have 2500 PGM in stake or more ]
5000 PGM IN STAKE = 2x rewards!
Discord
Support the curation account @ pgm-curator with a delegation 10 HP - 50 HP - 100 HP - 500 HP - 1000 HP
Get potential votes from @ pgm-curator by paying in PGM, here is a guide
I'm a bot, if you want a hand ask @ zottone444
Muchas gracias amén, amén que así sea 🙏✨
Excelente contenido apropiado para registrar en la blockchain Doctora Gracias
Saludos @otrobeta que gusto tenerlo por acá. Agradecida por su valoración y comentario.
Feliz semana para tí y los tuyos.
!hivebits
Success! You mined 1.0 HBIT on Wusang: Isle of Blaq. | tools | wallet | discord | community | daily <><

And, you found a BLAQ pearl (BLAQ)!
Check your bonus treasure tokens by entering your username at an H-E explorer or take a look at your wallet.
Read about Hivebits (HBIT) or read the story of Wusang: Isle of Blaq.
PIZZA Holders sent $PIZZA tips in this post's comments:
@acgalarza(1/5) tipped @marilour (x1)
Join us in Discord!
We appreciate your sharing of the vast knowledge of Cancer and as it concerns prostate cancer @marilour . It's great to have professionals like you educating us on what is needful.
A question for your consideration Ma?
Does frequent or no sexual activity reduce or increase the risk of prostate cancer?
Thank you for participating in this HEALTH WEEKLY DISCUSSION. The MED-HIVE community is grateful for your contribution on our primary goal of bringing health awareness to Hive.
We hope to grow more with your help and support!
Please consider supporting the med-hive community by subscribing and joining our Discord Channel. You can also go the extra mile and follow our voting trail, give this comment an upvote or even make HP delegations to the @med-hive account using the links bellow100HP|250HP|500HP|1000HP

Use Ecency! Did you know you can earn Ecency Points just for your regular Hive activity such as posting, doing comments, and upvotes? Use those points to boost and promote your or others’ hivers posts. You can even tip your favourite authors directly! How cool is that?!
Greetings @med-hive thank you very much for such kind words. I sincerely appreciate it. Thank you @ecency for the points, happy.
Regarding the question:
It is very interesting and I express the following considerations to you:
-Bearing in mind the relationship of the prostate with sexual activity, in the search for factors that may contribute to the prevention of prostate cancer; sexual behavior has been studied.
In this regard, scientific research has been conducted, of them there is a 2016 study, published in a widely accepted scientific journal European Association of Urology:
Ejaculation Frequency and Risk of Prostate Cancer: Updated Results with an Additional Decade of Follow-up. Rider y cols.
The study included 31925 men who answered questions about ejaculation frequency in a questionnaire in 1992 and continued until 2010. The evidence suggests that ejaculatory frequency may be inversely related to prostate cancer risk. It concludes by expressing the benefit of ejaculation in the prevention of prostate cancer.
My opinion:
-Studies conducted have been based on surveys, where respondent-dependent false answers may be generated.
-Other factors such as physical activity, diet, etc. should be considered.
-Research should continue to obtain more conclusive results.
-However, sexual activity (ejaculatory activity) through intercourse or masturbation is usually beneficial and favorable for men.
Hi @marilour.
I like the answer, not only that you mention the survey-based research, but your appreciation about the "errors" in it. Also the fact that you suggest to follow it up, maybe even applying other instruments.
Then you mention that indeed "ejaculation" benefits the man. Now how or why?
I know friends (men and women) who - in my non-professional judgment - are addicted to masturbation and express it normally. In short, they see it as a way of releasing tension....
And another question I have asked myself and wish to know is whether there is an (average) age for human beings, at which it can be said that the body is fully mature and in the best conditions to initiate sexual relations?
I ask you that, because among pets, specifically dogs, it is recommended not to mate them before the age of two, to let their body fully develop. So for us, when?
Greetings and blessings.
Hi @alummno, it's a pleasure to have you around, thanks for reading and joining the discussion with your interesting questions.
As you refer my opinions are conjectures and appreciations that may or may not be true, accepted or not by peers and the scientific community.
-Yes, in general, ejaculatory activity is beneficial to men's health in several aspects: it improves the quality and quantity of sperm, has a relaxing effect, excites the virile member, helps men become familiar with their sensations and needs, among others.
-The theory under study, ejaculatory activity-prostate cancer, is based on the fact that it releases accumulated prostatic fluid, the retention of which could have "carcinogenic" effects (under study).
-However, if any beneficial action is distorted, conditioning it to abuse and/or excess, it could generate the boomerang effect, becoming harmful. Addiction" would perhaps be a pathological behavior.
Until another time.
Happy week.
Interesting
Wao! It's too soon.
I thought it took longer to mature.
Thanks for replying...
It is an average, and will also depend on particular factors. Nowadays, adolescents start sexual activity at an earlier age, hence the high frequency of unwanted pregnancies in adolescents, as it happens in my country Venezuela.
It was a pleasure, we are in contact.
Si, si. Descubrí que eras venezolana.
Y no es casual que te haya preguntado eso, pues el objetivo es tocar el tema en un programa de radio con motivo de contribuir a la educación sexual y establecer los riesgos y responsabilidades que conlleva tener relaciones sexuales y lo complicado de iniciar a temprana edad.
Pues, quizá tengas datos estadísticos, y aprovecho para preguntarte si ese factor, de precocidad sexual, está directamente relacionado con el cáncer a nivel genital femenino a temprana edad (-40 años).
Yes, yes. I found out you were Venezuelan.
And it is not by chance that I asked you that question, since the objective is to touch on the subject in a radio program to contribute to sex education and to establish the risks and responsibilities involved in having sex and how complicated it is to start at an early age.
Well, perhaps you have statistical data, and I would like to take this opportunity to ask you if this factor of sexual precocity is directly related to female genital cancer at an early age (-40 years old).
Excelente 👋 😊 🇻🇪 "paisano", ya te envío material informativo. Quizás pueda serte de apoyo referencial.
Educación de la sexualidad y salud sexual y reproductiva.Fondo de Población de Naciones Unidas, Venezuela. 2010
Comportamientos sexuales riesgosos y factores asociados entre estudiantes universitarios en Barranquilla, Colombia, 2019. Badillo-Viloria y cols.
Estamos para servirte, cualquier cosa envía un mensaje y ahí estaré. Ten presente que debes referenciar siempre de donde obtienes la información (fuente).
Éxitos en tu actividad 👏 🙌 ✨
Ciertamente. Gracias por ser linda y recordármelo.
Gracias, de verdad gracias.
Está interesante el material.
Voy a revisar
Excelente publicación @marilour. Últimamente he visto a muchos vecinos caer por el cáncer de próstata, casualmente el año pasado murieron 2 uno enero y otro en febrero por dicho cáncer. Uno de ellos ya tenía años luchando, pero el otro si se vió más grave por no hacerse los exámenes en el tiempo necesario, cuando accedió a hacerse las pruebas ya todo estaba muy avanzado, lo que más impacta es el cambio físico en poco tiempo que llegan a tener, sobre todo la pérdida de peso.
Siempre he leído que la edad en la que más recomiendan hacer seguimiento a temas prostáticos es a partir de los 40, como lo mencionas en este post, pero ¿no sería recomendable iniciar el proceso antes? Un abrazo y gracias por compartir estos post.
Saludos @abneagro gracias por unirse a la tertulia discursiva, sobre el cáncer de próstata. Gracias por compartir tu experiencia al respecto. Según lo que refieres, ambas situaciones fueron de torpe evolución y mal pronóstico. Sí, a veces ocurre.
En cuanto a su pregunta asociada al grupo de edad, con su sugerencia de menos de 40 años para pesquisas. Realmente no tengo respuesta. En nuestra ciencia, la medicina, el establecimiento de parámetros por grupos de edad para las condiciones de salud, son resultados de la investigación científica (estudios longitudinales, meta-análisis y / o ensayos clínicos controlados) y las estadísticas registradas de los procesos de morbilidad (enfermedad) la mortalidad (muerte) por enfermedad, en las entidades que rigen las políticas de salud.
La investigación no se detiene y el cáncer de próstata sigue siendo el cáncer más frecuente en los hombres. Si nuevas investigaciones informan que el tamizaje debe iniciarse en edades menores de 40 años, así será y en consecuencia se generará una política mundial para su implementación.
Gracias por la socialización.
Salud y bienestar para Usted y los suyos.