Metabolism of Bilirubin and Jaundice
Hello everyone, it is good to have you here on my blog post today. Today, I will be writing about a bilirubin condition known as jaundice. I remember some years ago, my aunt spent nights at the Lagos State University Teaching Hospital (LASUTH), because my baby cousin had jaundice. She was very worried and at a point, I stopped worrying about the child but for her. At the end, the child received a blood transfusion, and other treatment, and over time, we were back home.
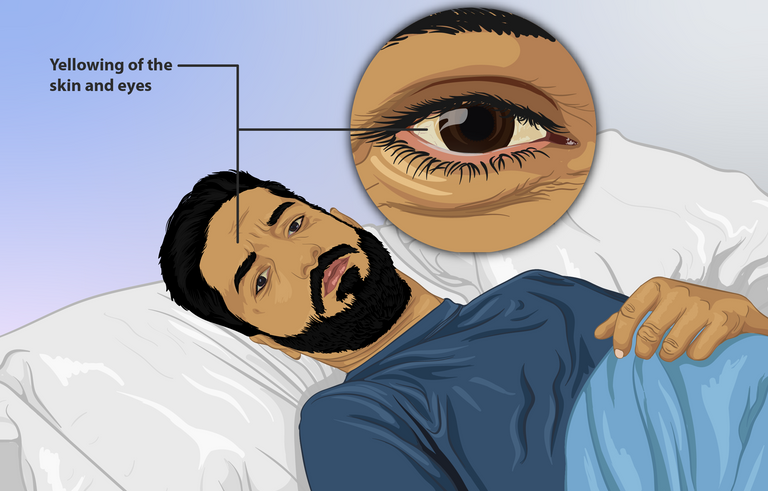
commons.wikimedia.org - Depiction of a jaundice patient
Metabolism of Bilirubin
Jaundice! A medical condition associated with excessive Bilirubin accumulation in the blood, causing the yellowing of the skin, sclera and mucous membrane. To understand jaundice, we need to get a clear view on what bilirubin is. Bilirubin is the oxidized/degraded form of heme (Hemoglobin) which makes up 70%, and from Myoglobin (a heme protein). The blood after 120 days becomes rigid and unable to squeeze itself into capillaries and narrow blood vessels, thereby leading to its death. This occurs when the old red blood cells move in through the spleen, the liver, and bone marrow, macrophages comes to engulf them. When the blood cell is engulfed, the amino acid in the globin of the red blood cell is reutilized in the body where needed, and the Heme is metabolized. The metabolized heme is turned into Biliverdin through heme-oxygenase. (Biliverdin is always excreted in reptiles, but it is not in mammals).
The Biliverdin cannot cross the blood-placenta barrier, in babies and excessive Biliverdin will lead to hyperbiliverdinemia which lead to a greenish coloration (jaundice) of the skin. To prevent excessive biliverdin, it is converted to bilirubin through the biliverdin reductase enzyme. Bilirubin goes into the bloodstream and moves through the bloodstream through albumin and moves to the liver. In the liver, the albumin is seperated from the bilirubin. Humans make an average of 250mg/day to 350mg/day at 1.5mg/dl in the blood. The Bilirubin becomes UDP-glucurinosyltransferase making it water-soluble, as a conjugated bilirubin which is sent to the gall bladder to mix with bile which helps to emulsify fat. The Bile is sent to the large intestine, where bilirubin is metabolized into urobilinogen, then to stercobilin where it is excreted with fecal matter. It is responsible for the brownish color of feaces. Majority of the bilirubin in human is excreted as waste, thereby not causing excessive amount of bile in the body. The rest is sent to the kidney where it is converted to urobilin, where it is excreted via urination, also, part of the bilirubin is sent to the liver where it restarts the enterohepatic circulation.
Jaundice
Jaundice is as a result of hyperbilirubinemia, which causes the yellowing of the skin, mucus membrane and the sclera of the eye. In newborn, Jaundice can occur as a result of certain conditions, which includes; the Crigler-Najjar syndrome, where the liver can't break down bilirubin, as a result of a mutation in the gene that encodes UDP-glucurinosyltransferase, causing unconjugated bilirubin to accumulate in the blood. Another condition is the Gilbert syndrome, which also causes accumulation of billirubin in the blood. The Dubin-Johnson syndrome is another syndrome which is caused by a mutation in MRP2, thereby not exporting conjugated bilirubin to the gall bladder, and Rotor Syndrome which is the accumulation of conjugated and unconjugated bilirubin in the blood.
Pre-Hepatic Jaundice has the hyperbilirubinemia occurring before the liver. This could occur as a result of several conditions, such as over production of red blood cells (hematopoisis) which would result in polycythemia. It could also occur during hemolysis process, where the red blood cell is broken down before the right time. This could also be in cases such as sickle cell anemia, cases of hematoma, also, production of Rhesus antibodies due to Rh differences from mother to infant causing hemolysis, and also cases where the blood is destroyed due to blood incompatibility from blood transfusion. Also, in cases where albumin is not attached to the bilirubin, it would lead to a hyperbiliverdinemia before the liver. Excessive use of antibiotics such as sulfonamide could lead to the hyperbiliverdinemia causing jaundice. Unconjucated bilirubin can also cause neurological toxicity conditions such as kernicterus (in infants). It is important to know that in pre hepatic jaundice, unconjugated bilirubin is responsible for jaundice.
Jaundice could also occur in intra-hepatic causes. This is when the liver itself is damaged. Hepatocellular causes of jaudice could be Viral Hepatitis, Fatty-liver diseases, liver tumors, and metabolic diseases. Jaundice could occur as a result of Post-Hepatic causes. These conditions occur after the bilirubin leaves the liver. These areas are the gall bladder, and the bile duct. Conditions such as Cholestasis, gall stone, tumor in the gall bladder can cause jaundice.
Condition
Jaundice in adult doesn't require treatment in adult, treating the cause of the jaundice is a good way to treat jaundice. In infants, it can be a serious problem and should be treated immediately.
National Library of Medicine - Hyperbiliverdinemia
Science direct - Bilirubin Metabolism
National Library of Medicine -Crigler Najjar Syndrome
National Library of Medicine - Dubin Johnson Syndrome
The Mechanism of Enterohepatic Circulation in the Formation of Gallstone Disease
National Library of Medicine - Jaundice
Medcomic.com - Types of Jaundice
Yay! 🤗
Your content has been boosted with Ecency Points, by @bimbo45.
Use Ecency daily to boost your growth on platform!
Support Ecency
Vote for new Proposal
Delegate HP and earn more
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.