Hydroxychloroquine and Vision Loss
People value their eyesight and fear blindness, in many cases more than they fear other forms of disability. It is this importance most of us place on eyesight that prompted me to write this blog about hydroxychloroquine and its association with vision loss.
One of the first instructions a physician will give a patient at the beginning of hydroxychloroquine therapy is, get your eyes checked. From the earliest days of this drug's use (for lupus, and other conditions) a recognized side effect has been irreversible and even progressive damage to the retina. This insult to the eyes is referred to as hydroxychloroquine toxicity. What I'll try to share with readers in this blog is the current thinking about potential damage to the eye from hydroxychloroqine, and the most recent safety guidelines for use of this essential drug (according to WHO's 2019 Model List of Essential Medicines).

Hydroxychloroquine and Eye Damage

Photos, credit: NIH, public domain
The photo on the left shows a typical 'bull's eye' retinopathy (disease of the retina), as it affects the field of vision. While the image on the left represents the clinical presentation of a patient with macular degeneration, this pattern is similar to vision loss experienced by people with hydroxychloroquine retinopathy, according to an article in the British Journal of Ophthamology. Quoting from the article: "In addition to HCQ toxicity, the differential diagnoses for bull's eye retinopathy include (s) macular degeneration."

Most people have become aware of hydroxychloroquine because of its possible therapeutic value in treating COVID-19. However, anyone with lupus is probably familiar with this drug, although it may be dispensed under another name. Two major brand names are Plaquenil and Quinoric.

To tell the story of hydroxychloroquine we have to go all the way back to pre-Columbian Peru. This is where the bark of the Cinchona tree was used to treat people who suffered from chills and fever. The bark was exported to Europe, where by 1820, quinine was isolated and used as an anti-malarial.
The Cinchona Plant

Photo by David J. Stang CC 4.0 license*

In 1934 chloroquine was synthesized, and in 1950, hydrochloroquine was synthesized. In each case, formulation of the drug evolved to eliminate some of the serious side effects.

Formulas for Hydroxychloroquine, Chloroquine and Quinine
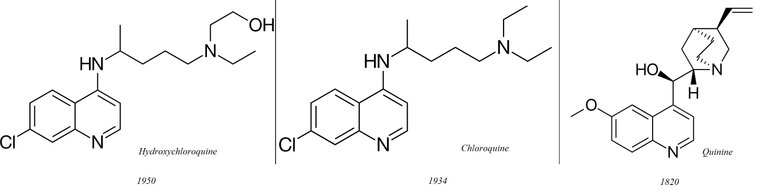
Public domain images:(they are simple structural formulas, ineligible for copyright and consist entirely of information that is common property and contain no original authorship.) Hydroxychloroquine formula: Fvasconcellos, Quinine formula: Vaccinationist, Chloroquine formula: Fvasconcellos

Hydroxychloroquine for Lupus
The U. S. Food and Drug Administration first approved hydroxychloroquine for treatment of lupus in 1956. However, anti-malarials (quninine and quinine-like drugs) had been used as far back as 1894 to treat different forms of lupus.
Looking back at articles published in 1999, in the Journal of Rheumatology concern is expressed about damage to the retina from long-term hydroxychloroquine use--that is, a period as long as six years. Most patients who are prescribed this drug traditionally have been advised to get an eye screening before beginning therapy. They've been told they should get another screening after six months, or at least at the end of one year. It is then recommended that they follow up with regular eye exams.
A 2006 study, Early Paracentral Visual Field Loss in Patients Taking Hydroxychloroquine, published in JAMA Opthamology, confirms the concern for retinal damage, damage that is often undetected until harm has been done. The JAMA article concludes: "visual field testing shows that visual field defects appeared before any corresponding changes in any other tested clinical parameters".

A Retinal Camera
User: Jason 7825, CC 3.0,2.5,2.0,1.0
A retinal camera is used to detect changes in the retina.

Another article, published in 2016, Retinal Toxicity in Patients Treated With Hydroxychloroquine: A Cross-Sectional Study, in Medical Hypothesis, Discovery & Innovation Ophthalmology, describes the eye damage detected in patients taking hydroxychloroquine. This article points out that there are certain risk factors which increase the likelihood a patient will experience hydroxychloroquine toxicity: "advanced age, use of a higher cumulative HCQ dose, and a longer duration of treatment".

Amsler Grid for Earlier Detection of Hydroxychloroquine Toxicity
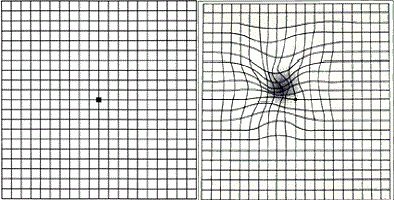
Image Credit: U.S. gov't public domain
According to the British Journal of Ophthalmology (2005), the Amsler Grid is one of the tools ophthalmologists use to screen for early (asymptomatic) damage to the retina. This is a grid that patients may use at home as a rough indication of whether or not they are suffering some loss in the visual field. The grid on the left reflects a normal field of vision. The grid on the right shows how the grid might appear to someone suffering macular damage. A patient would be instructed to visit the ophthalmologist as soon as the lines on the Amsler Grid appear curved. A cautionary note about the reliability of the test, especially in patients with long-standing vision loss: patients may automatically 'fill in' (think that they see) spaces and therefore give an inaccurate reading.
One of the early changes detected by ophthalmologists in screening for hydroxychloroquine toxicity is a change in color perception. This abnormality may be detectable even before other damage is evident. The authors of an article, *Detecting Chloroquine Retinopathy: Electro-oculogram Versus Colour Vision, in the British Journal of Ophthamology, (2003) state: "...screening for chloroquine retinopathy can be improved by using a sensitive colour test. Disturbance of the tritan axis appears to occur first. A normal test result on computerised colour testing virtually excludes any retinopathy by antimalarials."

The Most Recent Thinking on Hydroxychloroquine and Eye Care
An article (March, 2020) published in Covalent Careers, a journal for eye care professionals, outlines the current standard of care recommended by the American Academy of Ophthalmology. The AAO suggests that before the drug regimen begins, the patient should undergo an eye screening to determine if there is pre-existing maculopathy (disease of the macula). This article suggests that a patient wait a year for a recheck. I have read that a recheck should occur sooner than that. Although the risk of damage in the first year is slight (about 1% by some estimates), it does exist. However, I have read sources that place the risk higher than 1%.

Ishihara Plate, Used to Detect Color Blindness
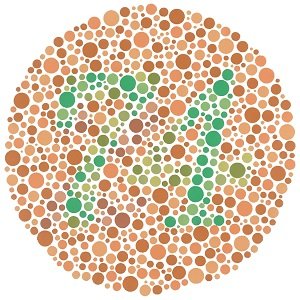
Image Credit:Unknown source. Public domain "because it consists entirely of information that is common property and contains no original authorship."

Risk Factors
Eye damage may more likely occur in people with the following risk factors: The factors cited by the AAO are presence of other therapeutic drugs (tamoxifen was mentioned specifically), kidney disease, liver disease, age and certain genetic factors. To minimize risk of toxicity the AAO suggests keeping the daily dose below 5.0 mg per kilogram of body weight. Keep in mind that once the damage has occurred, it cannot be reversed. For this reason, hydroxychloroquine must be discontinued at the earliest sign of toxicity.
Eye Damage in a Patient After Short-term Use
Although the guidelines for monitoring damage typically describe a one-year time frame, it should be noted that exceptions to this exist. An article in Ochsner (2017), Highly Accelerated Onset of Hydroxychloroquine Macular Retinopathy, describes the case of a 61-year old woman who was prescribed the drug for rheumatoid arthritis. After two months she suffered vision loss and was found to have a classic, hydroxychloroquine-associated bull's eye retinopathy. This represents central vision loss. The 61-year old patient had undergone retinal screening before beginning hydroxychloroquine therapy and at that time was found to have no retinal disease.

Damage May Occur Even When Hydroxychloroquine Is Discontinued
It is important to note that even when the drug is discontinued because of retinopathy, damage to the retina is not only irreversible, but it may continue. In the case cited above, the disease did not progress, although the damage was irreversible. However, a 2011 article published in an American Academy of Ophthalmology journal reports the existence of, "persistent toxicity after discontinuation of the medication." It is believed this may occur because the drug accumulates in tissue and remains in tissue after discontinuation of therapy.
A Right and Left Eye, with the Macula at the Center: No Macular Pathology
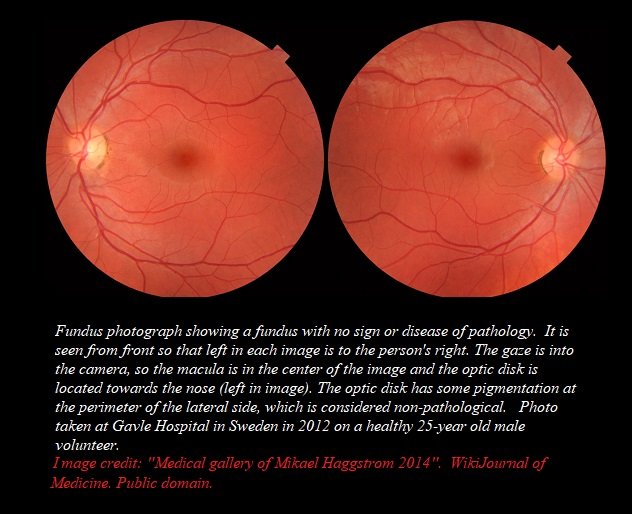

Asian and Caucasian Patients Show Different Manifestations of Hydroxychloroquine Toxicity
An interesting point of information in the AAO guidelines is that the pattern of ocular damage may vary in different populations. In Asians damage may occur outside of the macula, as well as inside the macula. An article published by StatsPearl in 2020 explained that 50% of Asian patients who suffered retinal damage showed a "pericentral maculopathy without the classic parafoveal (Bull's eye) retinopathy". Only 2% of Caucasian patients showed this pattern. It is suggested that the visual field test for Asian patients be adapted to accommodate this variation.

Conclusion
I know this blog has a lot of technical terms, but I think it's important that people have tools to make informed decisions about prescribed medications. Hydroxychloroquine is a wonderful drug. Studies show that lupus patients who take the drug for many years, and even for a lifetime, live longer, on the average, than lupus patients who don't take it. Hydroxychloroquine helps to limit damage to the kidneys and the nervous system. However, if I were to take this drug I would become very familiar with my ophthalmologist and I would make sure the most sensitive, early detection screening tools were used to detect pathology.
Also, eye damage is not the the only side effect a patient may experience with hydroxychloroquine. A list of other side effects may be found here.
Thank you for reading my blog. I wish everyone good health. Hive on!



Some Sources Used in Writing This Blog
- JAMA Ophthalmology Public Attitudes About Eye and Vision Health
- WHO Model List of Essential Medicines
- British Journal of Ophthalmology
- Montana Public Radio: [Cinchona[(https://www.mtpr.org/post/cinchona)
- Malaria Journal
- Medicines for Malaria Venture
- ACS.org: Molecule of the Week
- Lupus.org: Spotlight on Hydroxychloroquine
- Archives of Dermatology Response to Antimalarials in Cutaneous Lupus Erythematosus A Prospective Analysis
- Journal of Rheumatology: [Discontinuation of antimalarial drugs in systemic lupus erythematosus]
(https://www.ncbi.nlm.nih.gov/pubmed/10229401) - JAMA Network: Ophthalmology
- Medical Hypothesis, Discovery & Innovation Ophthalmology: Retinal Toxicity in Patients Treated With Hydroxychloroquine: A Cross-Sectional Study
- British Journal of Ophthalmology: Threshold Amsler grid as a screening tool for asymptomatic patients on hydroxychloroquine therapy
- All About Vision: Amsler Grid
- Science Direct: Occupational Therapy with Aging Adults
- British Journal of Ophthalmology: Detecting chloroquine retinopathy: electro-oculogram versus colour vision
- Covalent Careers: Opthalmologists, Plaquenil, Coronavirus
- Colormax: Color Blind Test
- Eyewiki: Hydroxychloroquine
- Breast Cancer.org: Tamoxifen
- The Ochsner Journal: Highly Accelerated Onset of Hydroxychloroquine Macular Retinopathy
- American Academy of Ophthalmology: Hydroxychloroquine-Induced Retinal Toxicity
- American Academy of Ophthalmology: Revised Recommendations on Screening Chloroquine
- StatPearls: Chloroquine And Hydroxychloroquine Toxicity
- Johns Hopkins: Lupus Treatment
- Drugs.com: Hydroxychloroquine
Shared on Twitter
Very informative, and great research on Hydroxychloroquine, thank you.
Do you know any good studies or results from Hydroxychloroquine in combination with zpak or zinc to treat Covid-19?
And, is it true that quinine can be also found in regular store "Tonic Water"?
upvote and follow.
Thank you for those kind words. Great questions! I will look that up (I love doing research) and find out if there are studies that show the effect a zpak or zinc/hydroxychloroquine combination may have. I'm pretty sure that the data with reference to COVID19 will be unreliable, because the history is so short.
I will edit this response later as I learn (or don't learn) about these combinations.
Follow back :)
Yes, great point at this stage it is too early for a good reliable study on almost any therapy.
Netherless, Boris Johnson and other famous people have been successfully treated with HCQ + Zinc.
But, I guess only time will tell and I would definitely appreciate your further research, thank you.
https://www.zerohedge.com/political/association-american-physicians-says-trump-touted-drug-has-90-chance-helping-covid-19
Hi,
Thanks for that link. I went to sleep last night reading about hydroxychloroquine, zinc and zithromax (no nightmares, though 😄). One of your questions is easy to answer: yes, tonic water does have quinine. As for the therapeutic value/safety of the other drug combinations: not so easy. Now that the drug combination has become a topic of political discussion, I have to look back at pre-COVID19 to get objective information. I'm still reading, and so far found some interesting details. All three drugs alone are associated with negative cardiac events. Here are three articles: ZPAC, hydroxychloroquine, and zinc. Not surprisingly, (given the individual effect each drug has) cardiac complications have been noted in people who take a combination of the drugs. Whether or not the drug combinations are effective treatments for COVID--this is such a political hot potato. Time will have to pass and valid, control studies done, in order to evaluate the efficacy of the drug combination in treating COVID. I think we may be looking at development of an antiviral(remdesivir) in the near future. This has apparently been looked at in at least one rigorous study.
Let's hope so.
Thank you for sending me into these corners of the science universe to find answers. Hope you enjoy good health and never have to personally find out if these medicines work :)
This is an excellent article - as expected.
This shows a not very well understood problem. Even most academics don´t get this. It is called non-ergodicity.
Russian roulette: - a 10000-chamber revolver and only one bullet. You can win what ever you wish. For you, it is very unlikely that you catch a bullet and for a super-majority of people it is also very unlikely that they catch a bullet. If the ensemble is big enough some will die. All in all the upside for the population is massive.
For the individual, a non zero probability of an irreversible loss aka ruin is something which should make clear - >>don´t take this bet<<. From the individual perspective NO One should take it <--> from the ensemble perspective everyone should take it.
I mean, Covid looks like a nail and hydroxychloroquine is a hammer. Lupus is a nail, malaria is a nail, Covid looks like a nail. When you don´t take it --> you die with >0 zero probability and when you take it, --> you loose your vision with >0 probability. Life>vision ...thats the normal logic behind medicine I guess.
However, often it is very easy and cheap to establish tissue selectivity and reduce off-target effects. Take chemo-therapy sessions: People say "hairs will grow back". Of course I would not think twice and take the therapy. But we know that during the short session it would be enough to simply cool down the scalp to 6°C/40°F...still no one uses this technique. And loosing your vision comes for most people right before losing your life...big pharma does not spend much money on compliance issues.
Have a great weekend!
Thank you for such high praise, @lauch3d. I have learned a new word, non-ergodicity. And you know I have looked it up:) Fascinating concept.
It maddens me, a bit anyway, that the recommendation is made for a first post-therapy check-up to take place one year after commencement. If people knew what they were risking...
Cost-benefit calculation? To the individual practitioner, or to the healthcare system?
I like to encourage people to question, and to investigate (and not just in healthcare). I think it's a basic survival tool.
You stay well and continue to dazzle with your amazing analytic skill.
Warm regards,
AG
A couple of days ago I was watching this announcement by Dr. Fauci. Afterwards I scrolled through the comment section (as I'm always interested in getting to know people's views) and came across the following comment:
My goodness, the story we tell ourselves. The extent to which we (humans) willingly (?) reshape reality to fit it within the framework of our own beliefs.
Personally, I had never heard of this medication before this entire COVID-19 nightmare. Your article brings incredibly important, but also terrifying information. Patients arriving at a hospital under critical conditions have no time to have their eyes checked before being medicated. Stories like the 61 year-old lady who lost her vision as a side effect of a treatment is simply heart-breaking :/ Yet, we find ourselves in a situation where major world authorities push people to try this drug while asking "what do you have to lose?".
As @launch3d observed, this is an excellent article - as expected! :) Highlighting the reasons underlying why damage might persist even after hydroxicloroquine therapy is interrupted (due to accumulation in the tissues), brought further thoroughness to your work.
Your scientific writings never fail to impress me my dear friend.
I trust you, your husband and children are healthy and safe over there in NY.
Much love to you from sunny, warm Portugal <3 :*
Hello dear Abigail,
So nice to see you here. Thank you for the kind words. I think you and I share frustration over the conflation of science and opinion. Really important decisions are corrupted by emotional response to one political view or another. Finding objective answers is hard enough even with proper study. When emotions enter the equation, there is just a muddle.
I hope the virus has spared you and yours. It has spared my family, so far, although it has taken at least one friend and few distant acquaintances. New York seems to be the St. Giles in the Fields of the COVID pandemic. It's kind of surreal being here.
Please be well in sunny Portugal. Again, it was very good to hear from you.
With great affection,
AG
I'm very sorry about your friend @agmoore :( How sad. This, indeed, is a testing time in our lives. My sister-in-law and my brother have tested positive. My sister-in-law has been feeling a little poorly over the past few days (she is at home) and my brother has presented virtually no symptoms.
Please take care my dear friend.
My thoughts go to you and the families of those you've lost.
With infinite love from Portugal.
I'm so sorry about your family. I read last night that Portugal has a higher incidence than I thought. Please be safe. I wish your brother and sister-in-law complete and speedy recovery.
Love from your friend in New York,
AG
Hey Agmoore,
we are living in crazy times. That's all I can say about this.
Excellent article again, re-hive, enjoy!
Chapper
Hi Chapper,
Yes, crazy times. I hope you and your loved ones are well in these crazy times.
Thank you for your support. When I meet your standards, makes me smile--a lot :)
Regards, AG
You always meet my standards, thank you for your work.
Stay healthy and happy
Regards
Chapper
:)
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @steemstem account (for some ROI).
Please consider using the STEMsocial app app and including @steemstem as a beneficiary to get a stronger support.
Thank you STEMsocial! I love the new logo. I have named STEMsocial as beneficiary, but couldn't get the editor to work when I posted. So that's why this appears on my blog.
Health to all on the team!
From my point of view the chloroquine retinopathy is less important in a life threating diseases event like COVID-19.
Of course the retinopathy is an important side effect, but you has to screen a lot of patients in order to detect one case.
Amsler Grid and Ishihara in self care management and regular intervals of opthalmic control are necessary in a longterm therapy or if you use it as chemoprophylaxis.
However - we have to see what clinical results HQ will produce in the COVID-9 background.
Best regards.
!COFFEEA
Thank you very much for your feedback. I agree with your statement--this drug is useful, even vital for many people, in ways perhaps we have not yet discovered. My post is not directed against the drug, but against dispensing it to patients who do not fully understand the risk. Doctors tend to operate from a position of authority and patients tend to accept that authority. Patients should be active participants in their care. Patients should decide if the risk/benefit ratio is acceptable. Once the decision is made, patients should be armed with information so they can defend themselves (as much as possible) against a negative outcome.
The philosophy that drives my articles about healthcare: in every decision a doctor makes, the patient has more to gain and lose than the doctor. Therefore, the patient should be fully engaged in the decision-making process.
I very much enjoy your in-depth articles. Sometimes the information is challenging, but always I learn something.
Warm regards,
AG
I actually didn't know anything about what you presented here. I am really happy to have read your text!
Here, I am just so shocked about so many people mentioning this as a covid-19 treatment, moving on with paranoia with this professor being muted, etc... although studies are on-going (this seems to be absent from the media noise), most results seem to show there is no gain in taking it (this is also quite absent from the media noise), and so on (not discussing most side effects associated with the treatment). A lot of disinformation on this matter, IMHO...
I will advertise your blog to some ;)
Hi @lemouth,
Thanks so much for those words of support. Yes, it is dangerous and frustrating when science is muddled by politics. It's hard enough to get good answers from valid studies (we know these often contradict each other), but when misinformation is deliberately spread--that's dangerous.
As for the side effects of this drug: everything we take has a cost. That's just a fact. Not all of us have to pay that price, but some are negatively affected. Usually, doctors make a decision about the risk. I think patients should be able to participate in the decision, but they need information to do that. Every time I write a science article (as challenging as these are for me), I think my motivation is to arm people with information that they can use in every day life. Plus, I do love to write :))
Good health to you, your family and everyone we know (physically and virtually).
:)