Generalities and care of the use of analgesics, sedatives and relaxants in intensive care
On the other hand, critically ill patients present episodes of agitation during their stay in Intensive Care, developed by PTSD, mostly caused by pain, anxiety to the unknown, drug-induced hallucinations or traumatic pathologies at the cranial level.
These episodes of agitation lead to the patient removing the endotracheal tube, probes or catheters, increasing the risk of morbidity of the patient.
As a measure of providing the most humanized care possible to critical patients, the use of sedative agents, muscle relaxants and analgesics is required and these are among the most commonly used drugs in intensive care units.
The intensive care physician performs the pertinent calculations of these drugs to be used in the critical patient and the nurse specialist in the area proceeds to prepare it, and administer it taking into account the Right Five (Medication, dose, time, date and route of correct administration ) to avoid complications, with adequate cardiovascular monitoring and monitoring, detecting any eventuality and this with the main objective of achieving an improvement in pain, anxiety and sleep of the patient, as well as protecting the patient from self-aggression, or aggression to the team health, involuntary removal of tubes, drains, catheters and connections to the mechanical fan.
When starting the infusion of sedative to the critical patient through the continuous infusion pump or in bowling, it allows the specialist nurse to keep track of the pharmacological effect, allowing the patient to improve his ventilatory mechanics (fan tolerance), inadequate muscle activity decreases of the patient, allow tolerance to permissive hypercapnia if necessary, as well as reduce elevated intracranial pressure by reducing agitation and sympathetic stimulation.
The critical patient receiving sedative and relaxing drugs should be kept under cardiopulmonary monitoring, as well as secured the airway since the use of these can cause hypotension, bradycardia, hypoxia, oxygen desaturation, among others.

Public Domain Image
Benefits and unwanted effects in the use of sedation, analgesics and relaxants in the critically ill patient
The administration of sedatives and relaxants in the critical patient generates benefits that is why it is frequently used in these units among the main desired effects that facilitate therapeutic management we have to reduce hypertension, circulatory instability, oxygen consumption decreases and therefore the Cardiac requirements in patients with low-cost syndrome.
The sedative and relaxing agents used in the critical care units, as well as presenting a series of beneficial effects, can be manifested by many in an undesirable way among the most feared is circulatory depression, be it vasodilation or myocardial depression, depression can also occur respiratory, muscular atrophy, necrotizing myopathy, paralytic ileus, immobility in bed favoring the appearance of bedsores, retention of secretions, venous thrombosis, dependence or withdrawal from the drug.
Medicines most used in intensive therapy such as sedatives, relaxants and analgesics
There are many drugs used for sedation and analgesia in the critical patient allowing to facilitate the humanized care in these units by the doctor and the nurse among the most used sedatives we have midazolam, propofol, diazepam, ketamine in some cases and analgesics that favor To sedation are opioids and their derivatives such as fentanyl, morphine and tramadol, other non-steroidal anti-inflammatory analgesics can be used but these do not produce any hypnosis, these drugs can be administered both in bolus and in continuous infusions and this is where the Dosage dynamics administered according to the patient's response, with the use of scales and continuous cardiopulmonary monitoring.
When the patient who is under mechanical ventilation and his mandatory mode is fully developed by the apparatus and his orotracheal tube is free of secretions and present resistance to ventilation is required in many cases apart from using sedative and analgesic drugs with sedation effects the use of muscle relaxants and blockers such as vencuronium, pancuronium, rocuronium for total coupling to the mechanical ventilator.
Sedation, relaxation and analgesia is a primary point in the overall treatment of the critically ill patient especially when they are under mechanical ventilation, the administration of these drugs is for the purpose of controlling the hormonal response to stress (tachycardia, hypertension, hyperglycemia , increased protein catabolism) that is harmful to the patient. Similarly, sedoanalgesia allows an adequate coupling of the patient to the ventilator.
>We can say that the management of sedatives, relaxants and algesics in critically ill patients is aimed at controlling pain, decreased motor activity, amnesia, respiratory depression, which can facilitate mechanical ventilation and ultimately facilitate sleep.

Public Domain Image
Muscle relaxants
The use of relaxants is essential in the management of the patient connected to mechanical ventilation in controlled assisted mode, in control volume and in control pressure for proper coupling between the patient and the respirator.
To achieve relaxation of the patient at the central level, in the spinal cord (central muscle relaxants) and in the motor plate (peripheral muscle relaxants or neuromuscular blockers: healing), it will depend on the classification of these drugs in their place of action.
A.- Peripheral muscle relaxant drugs:
I.- Non-depolarizing:
D-Tubocurarin (Tucurin)
Galamina
Pancuronium (Pavulón)
Atracurium (Tracrium)
Vecuronium (Norcuron)
II.- Depolarizers:
Succinylcholine or Suxamethonium (Scoline)
B.- Central muscle relaxant drugs:
Methocarbamol (Robaxin, Robramol)
Carisoprodol (Soma, equilene)
Orphenadrine (Norflex)
Baclofen (Lioresal)
Dantrolene (Dantrium)
Chlorzoxazone (Paraflex)
Stiramate (Sinaxar)
Benzodiazepines, diazepam (Valium)
Mechanism of action of peripheral muscle relaxant drugs
D-Tubocurarin and the like (Paquicurares) act by competing with acetylcholine for the nicotinic receptor of the neuromuscular plate, preventing the depolarizing action of acetylcholine, which is why they are also called anti-depolarizing muscle relaxants.
The succinylcholine group (Leptocurars) act similarly to high doses of acetylcholine, bind to the receptor but cause depolarization, which is persistent and repolarization is prevented, the normal depolarization-repolarization sequence is blocked and new spreads are not propagated impulses, that is, there is loss of electrical excitability and after initial contractions (fasciculations) the muscle relaxes.
Pharmacological actions.
1.- Muscle relaxation
The d-tubocurarin (intravenous route) after 2 minutes of injection produces a flaccid paralysis, which is maximum in 5 minutes, and lasts on average, about 10 minutes. Succinylcholine produces fasciculations, prior to the onset of paralysis.
The first muscles to be paralyzed are the ocular ones, producing palpebral ptosis and diplopia, then the facial muscles, limbs, tongue and pharynx (Difficulty in chewing and swallowing). abdominal, intercostal, larynx and finally the diaphragm. Recovery is done in reverse.
Prolonged muscle paralysis can be observed in drugs that are metabolized by cholinesterase (eg succinylcholine) by genetic variants, 1 in 2000 people have cholinesterase genetic deficit.
2.- Circulatory system
Arterial hypotension may occur, which is explained by histamine release and lymph node blockage.
3.- Respiratory system
When diaphragm paralysis occurs, there may be respiratory arrest.
The release of histamine causes bronchoconstriction.
4.- Histamine release
It produces bronchospasm, hives and hypotension.
5.- Other effects
-All produce increased salivary and bronchial secretion.
-Positive potassium ion balance.
-Increased intraocular pressure
Pharmacokinetics
Absorption:
Oral absorption is almost nil. This is why they are administered via IV.
Distribution:
The pachychemurs are distributed in a limited way because of their high molecular weight and because they are derived from quaternary ammonium, they do not cross the blood brain barrier, nor do they penetrate the cell membrane.
Metabolism:
It is variable; d-tubocurarin is metabolized in 70%, in the liver by oxidation, others such as vecuronium is almost completely metabolized in the liver, succinylcholine is rapidly hydrolyzed by plasma cholinesterase, in two steps it is transformed into succinic acid and choline, atracurium is hydrolyzed spontaneously in the plasma, due to blood pH, some are almost completely eliminated in the urine without undergoing transformations, such as galamine and decametonium.
Adverse effects
Intoxication is produced by administration of high doses or by normal doses in hypersusceptible individuals, leading them in many cases to suffer:
1-Respiratory arrest
2-Bradycardia with succinylcholine and decametonium
3-Intense tachycardia with galamine
4-Other effects are arterial hypotension, histamine effects and hyperkalemia, with depolarizers, myalgia is observed in the postoperative period, the picture of malignant hyperthermia has been described, especially with succinylcholine-type drugs, which produces intense muscle spasm and a sudden increase in body temperature.
Clinical Uses
- They are used as muscle relaxants during surgical anesthesia or exploration under anesthesia, (Especially abdominal surgery, dental and traumatological surgery).
- Orthopedic or traumatic manipulations, reduction of fractures and dislocations, for endotracheal intubation, endoscopy, electroconvulsive therapy, diagnosis of myasthenia gravis, adjuvant tetanus therapy, encephalitis, poliomyelitis and seizure disorders.
Nursing Care
1.-Carefully monitored, especially breathing control, pulse and blood pressure.
2.-Monitor for adverse effects, apnea and hyperthermia.
3.- Have oxygen, neostigmine, atropine, adrenaline and a respirator available next to the patient.
4.- Aspirate bronchial secretions if dyspnea occurs if there is airway obstruction by them.
Sedatives and hypnotics
This group of drugs can be defined as substances that produce reversible depression of the central nervous system in a general and irregular way, causing varying degrees of effects, such as simple sedation (decreased psychomotor activity with decreased stress response), hypnosis or sleep, anesthesia, coma, respiratory depression and death.
Classification
Barbiturates and non-barbiturates
Barbiturates are divided into four groups according to the speed and duration of their effects:
Ultra Short Action
Thiopental
Metohexital
Short Action
Hexobarbital
Pentobarbital
Secobarbital
Intermediate Action
Amobarbital
Approbarbital
Butabarbital
Long Action
Barbital
Phenobarbital
Primidone
Pharmacological actions
1- Central nervous system:
Anticonvulsant action Barbiturates can increase pain, hyperalgesic action, Hypothalamic: decrease in temperature and blood pressure.
High doses can cause depression of the respiratory center.
2.- Cardiovascular system
Its use at therapeutic doses causes a slight decrease in blood pressure, high doses produce vasodilation due to central and peripheral effects with marked hypotension, vasomotor reflexes and cardiac contractility are depressed.
3.-Gastrointestinal tract:
Reduction of smooth muscle tone, with decreased motility and secretions, on the liver barbiturates, mainly phenobarbital, increased metabolic activity of hepatic microsomes, increase the conjugation of bilirubin with glucuronic acid. (Enzymatic induction) affecting microsomal and non-microsomal enzymes.
4.- Genitourinary tract:
1- The use of anesthetic doses decreases the strength and frequency of uterine contractions and depresses the contraction of the ureter and bladder.
2- On the kidney they produce decreased urine flow, in cases of intoxication severe oliguria or anuria occurs
Pharmacokinetics
Absorption:
Barbiturates are weak acids with high fat solubility.
Distribution:
It is broad, they bind albumin in varying degrees (Thiopental 65%, Secobarbital: 44% and phenobarbital and barbital: 2%). They cross the blood brain barrier and the placental barrier.
Elimination:
It is done by hepatic metabolization and urinary excretion in varying proportions, urinary elimination is affected by the pH of the urine.
Adverse effects
Centrals:
drowsiness, residual depression or hangover, paradoxical excitation and increased pain have been described,
you can also see vertigo,
Gastrointestinal:
nausea, vomiting or diarrhea
Hypersensitivity reactions: hives, angioedema, asthma and rarely exfoliative dermatitis.
Overdose:
It is characterized by varying degrees of depression of the nervous system, with respiratory and cardiovascular depression, hyporeflexia, oliguria, myosis that progresses to mydriasis as the coma deepens, there may be shock, apnea and death.
Indications and contraindications
a) As sedatives:
They are used very occasionally, because they have been displaced by minor tranquilizers.
b) As hypnotics:
Treatment of insomnia, for a short time, for example preoperative hypnotic (Preanesthesia)
c) As anesthetics:
Thiopental is used as an inducer of anesthesia or for short-term interventions.
d) Anticonvulsant:
Phenobarbital is mainly used as an antiepileptic, and in other seizures caused by eclampsia, tetanus, meningitis and intoxications (Strychnine, amphetamine local anesthetics.
e) Neuroprotectors
In postoperative patients of neurosurgery.
Non-barbiturate hypnotics
1.-Benzodiazepines:
Hypnotic Benzodiazepines:
Flurazepan (Fluralema)
Quazepam (Doral)
Temazepam (Restoril)
Triazolam (Halcinom)
Midazolam (Doricum)
2.- Non-benzodiazepine agonists:
Zolpidem (Stilnox)
Pharmacological actions
1-. Central Nervous System:
a) Anxiolytic action
b) Hypnotic or hypnoinductive action
c) Anticonvulsant action: diazepam, nitrazepam and clonazepam, intravenous diazepam is one of the most useful anticonvulsants today.
d) Antidepressant action: alprazolam
2.- Action on skeletal muscle, muscle relaxant effect:
Diazepam
3.- Cardiovascular system:
Discreet hypotensive action and decreased ventricular work, especially intravenously.
4.- Respiratory system.
The use of these drugs parenterally (IV) can cause a decrease in respiratory rate, rapid injection or high doses can cause apnea.
Mechanism of action
Benzodiazepines act by amplifying the inhibitory actions mediated by the neurotransmitter gamma aminobutyric acid (GABA) located in the neuronal membrane forming a macromolecular complex with the chlorine ionophore (Chlorine Channel). When the receptor is activated, the chlorine channel is opened with this ion entering the neuron and producing hyperpolarization / inhibition.
Anxiolytic action is produced because gabaergic facilitation translates into a decrease in serotonergic mechanisms in the Central Nervous System, the Rafe nucleus and the septo-hippocampal system.
Non-benzodiazepine agonist drugs are substances with different chemical structures than
benzodiazepines, but their effect is due to the fact that they stimulate the benzodiazepine receptor, joining the GABA receptor, its pharmacology is similar to that of benzodiazepines, produces little rebound and is considered to have low habituation.
Nursing care
1.-The hypnosedantes are one of the ways to calm the patient, you should not forget good nursing care and good patient-nurse communication
2.-Control of the environment in case of administration of hypnotics: reduce noise, listen to the patient and reduce their doubts and anguish, try to keep him awake during the day with some activities.
3.-If the cause of insomnia is pain, try to calm it and not use hypnotics for pain.
4.- Due to the depressing effect, the possibility of falls and other accidents increases, so the patient must be well monitored.
5.-Monitor for the presence of mental confusion or idiosyncratic reactions.
6.- When administering the hypnotic, monitor the onset of the effect. Be sure of ingestion, do not leave the medication with the patient due to the danger of automatisms and suicide attempts.
Public Domain Image
Opioid analgesics
These drugs, in addition to the analgesic action, have a sedative action, which is why they were also called
Hypnoanalgesics
Mechanism of action
Its action is due to the interaction with specific receptors (Mu μ, delta δ, Kappa κ, Sigma σ, Epsilon ε)
in the central nervous system (Brain, spinal cord) and peripheral nervous system.
According to this interaction they can be stimulants (Agonists), receptor blockers (Antagonists)
and with mixed action, agonist-antagonist (stimulation and blockage).
Pharmacological actions
Central Nervous System:
1.Analgesia Sedation, euphoria.
- Oculomotor nucleus stimulation (myosis)
3.Depression of the tumor center - Respiratory center depression (dose dependent)
- Stimulation Trigger Chemoreceptor Zone (Emetizing Effect)
- Center vomiting depression (antiemetic effect)
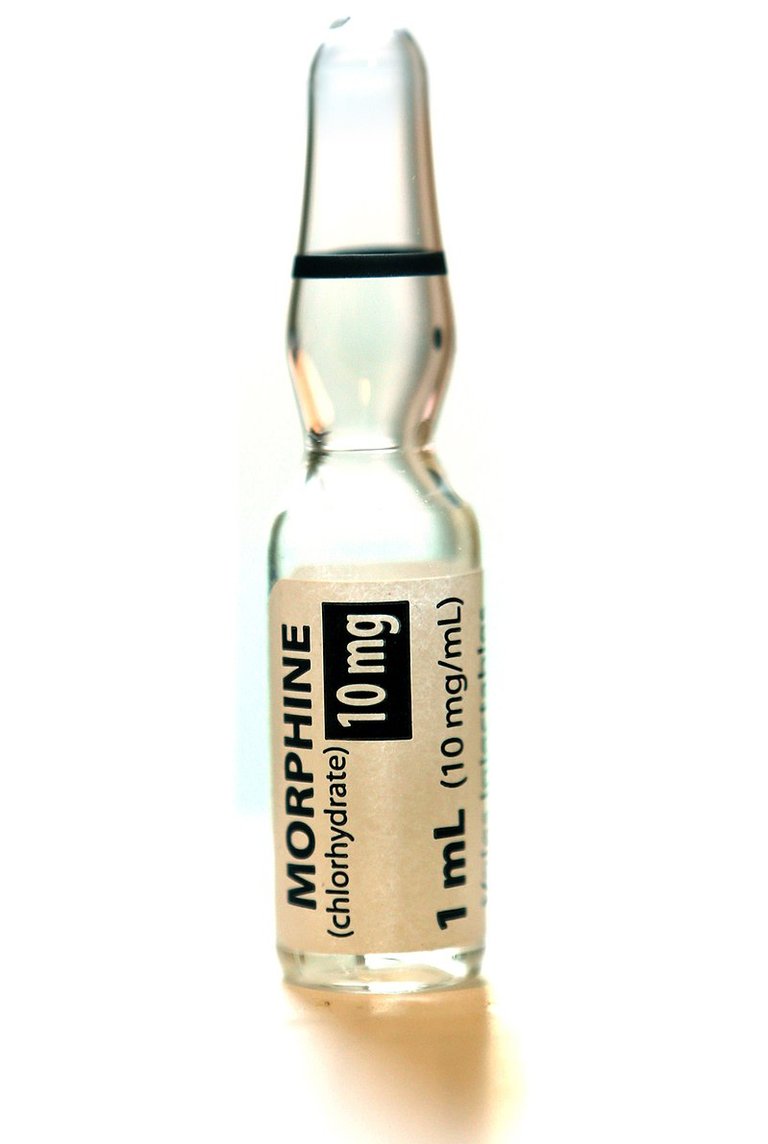
Morphine
It is the opioid with a longer half-life and duration of effects and these can accumulate if there is renal failure.
Meperidine
It is considered indicated in biliary and renal colic, pain of acute myocardial infarction with bradycardia and in the pain of acute pancreatitis.
Fentanyl
It is a potent synthetic opioid, with a shorter half-life and duration of effects.
Tramadol
Of the opioids it is considered the weakest. It is used in moderate pain, does not produce spasm of the sphincter of Oddy and respiratory depression is less frequent.
Indications
- Acute coronary pain.
2.Acute pulmonary edema
3, acute pancreatitis. - Acute peritonitis.
5.Biliary and renal colic
6 burns - Acute post-traumatic pain (Acute moderate to severe pain).
8 Vascular pain of ischemic origin - Migrainous status (Occasionally)
10.Acute cancer pain
Adverse effects
- Respiratory depression
2.Sedation. - Nausea and Vomiting.
- Decreased gastrointestinal transit, spasm of the sphincter of Oddy.
- Urinary retention.
Contraindications
- Respiratory function compromised.
2.Endocranial hypertension
3.Cranial trauma. - Bronchial asthma.
5.State of shock or hypotension
Nursing care
1.- Monitoring of side effects (Respiratory Depression)
2.- Monitor response to the administered dose
3.- Discuss with the patient: type of pain, anxiety fear of addiction (Use of pain)
4.- Monitor the appearance or development of dependence
5.- Postoperative abdominal pain, only if indicated.
6.- Do not give opioids as a substitute for nursing care used for pain.
References consulted
Reference 1
Reference 2
Reference 3
[Reference 4]https://aneskey.com/sedation-analgesia-and-muscle-relaxation-in-the-intensive-care-unit/)

I can't access the references. Only the last one and it is in Spanish. I recommend using references in English if the content is in this language, regardless of whether the content provided is from references in Spanish.
Greetings dear @ carloserp-2000, I will review what happened with the references used and thanks for your input.
Already fix what happened a hundred fails to access references