Subdural hematoma resulting from head trauma
In this opportunity I would like to share a very common topic in the area of medical emergencies that represents a complication due to a car accident, overturn, among others, which causes a head trauma that in turn the formation of a subdural hematoma.

Brain. By Staff Sgt. Joseph C. Hill, NCOIC, Behavioral Health Care Services, Aberdeen Proving GroundFebruary 12, 2015
A Subdural Hematoma is one that is formed when blood accumulates under the covering of the brain (called dura) and this usually comes from small vessels that have broken favoring the formation of small bags or sacs that protrude and make pressure, causing serious consequences. Based on the above, we say that when blood leaks from the veins and accumulates under the dura, it is called a subdural hematoma.
In the majority of patients with this brain injury, the antecedent is a traumatic brain injury, other cases of seizures, alcohol abuse, and coagulopathies.
According to its clinical presentation and evolution this can be acute, subacute and chronic, based on this, its symptoms and prognosis of the individual.
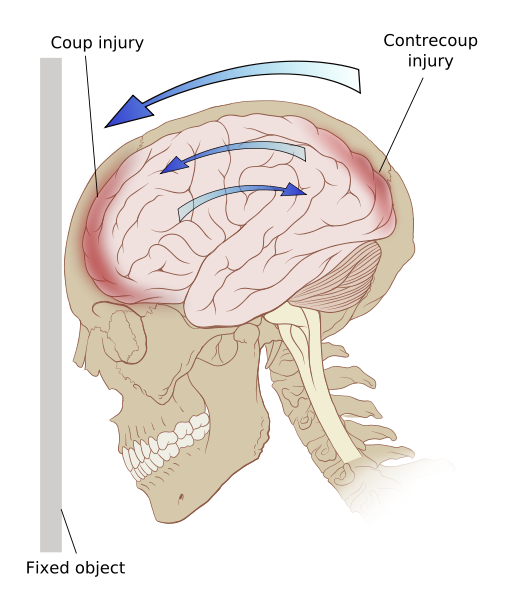
Traumatic Brain Injury. Public domain CC BY 2.5
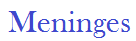
They are characterized by a set of membranes consisting of connective tissue that cover the central nervous system, whose objective is to provide protection to adjacent structures such as the bone (skull).
For its study, three layers and two intermediate spaces are described, therefore, we say from the inside out:
1. Piamadre, the innermost, thinnest, clearest and most vascularized layer, contains fibroblasts, being in close contact with the brain.
2. Subarachnoid space, contains the cerebrospinal fluid and its function is cushioning, corresponds to the space between the arachnoid and the pia mater.
3. Arachnoid, represents the intermediate meninge, located below the dura mater and is responsible for the distribution of the CSF.
4. Subdural space, virtual space between the dura mater and the arachnoid.
5. Duramadre, outer layer made up of a fibrous, thick and solid wall that allows its protective function.
The layers that make up the meninges have their specific functions of providing protection against both traumatic injuries (mechanical protection) that can endanger the life of the individual, on the other hand, provides protection against chemical attacks generating a barrier that acts as a filter for those external substances that want to penetrate the CNS injury.
Meningeal layers. Public domain CC BY 4.0
As just mentioned, this accumulation between the arachnoid and dura is what is known as a subdural hematoma.
It is classified according to its evolution:
This type of hematoma is more frequent than the epidural, and this could be due to the fact that it is the first exposed space (more external) that will receive the cranial contusion and therefore the first to be injured in comparison with the epidural hematoma.
Among the most frequent causes, as has been mentioned, 90% correspond to head trauma (TCE), which would represent traumatic aetiologies associated with head fractures. Spontaneous non-traumatic subdural hematomas are usually infrequent and associated with hematological pathologies (coagulopathies), infectious diseases, vascular malformations or hemorrhagic tumors.
Most often, these hematomas occur after a head trauma either from a fall, contusion, or other injury. Rarely, it may occur without a known cause. People with the following risk factors may be at increased risk:
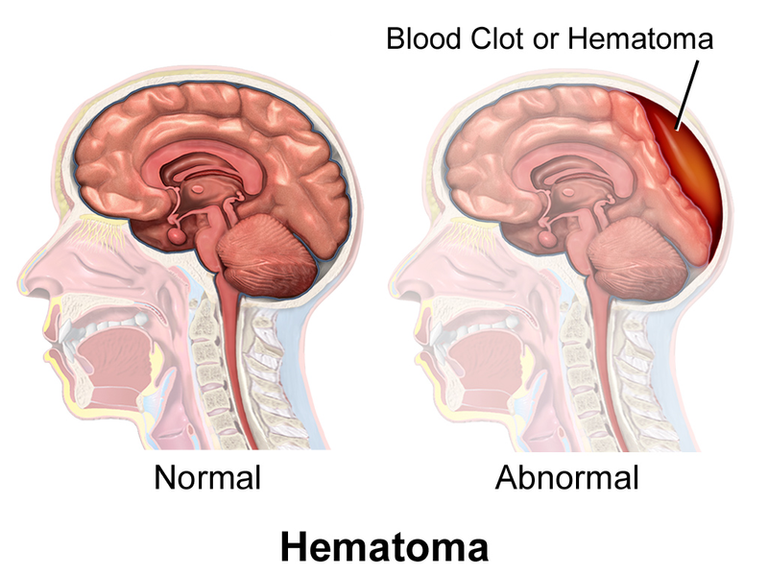
Hematoma Comparison. Public domain CC BY-SA 4.0

Characterized by a faster and more progressive clinic with installation in the first 24 to 72 hours after the traumatic event, in this case, once the venous rupture occurs, the bleeding does not stop, appearing a blood collection in the subdural space that increases in size quickly and progressively in a short time.
In 70% of the cases the patient may suffer from headache, nausea, vomiting and neurological focus.
Its clinical presentation is so acute, that it allows us to evidence even signs of neurological focus expressed in hemirapesia, dysarthria, deviation of the labial commissure, loss of consciousness, drowsiness, stupor, coma that can lead to death.
It occurs more frequently between the fifth and seventh decade of life, being more common in males than in females.
Two theories have been proposed for the development of chronic subdural hematomas:
The osmotic gradient theory.
The theory of recurrent haemorrhage from the haematoma capsule associated with hyperfibrinolysis is the most accepted, which is mediated by inflammatory and proliferative cellular factors that would act as predisposing factors for the alteration of local coagulation, and thus the formation and recurrence of bleeding in the subdural space.
Symptoms vary according to the location of the hematoma and may even be similar to a stroke clinic. Symptoms include.
Headache, Weakness or hemiparesis of some of the extremities. Loss of balance and/or coordination. Neurological alterations, e.g.: Changes in behavior, loss of memory, drowsiness, lethargy or coma. Loss of vision, dysarthria and seizures.
A subdural hematoma can be fatal resulting in death or permanent disability if not detected early.
The most feared complications include; Brain herniation and permanent brain damage.
The diagnostic abutment continues to be a good collection of data and background prior to the patient's current clinical picture that aids in diagnosis or diagnostic impression.
Physical examination, it is always recommended in these cases the exploration at skull level looking for the presence of stigmas, fractures that could explain neurological picture. As well as taking vital signs (blood pressure, respiratory heart rate and temperature) and of course perform a good neurological examination and determine the Glasgow scale that does not guide how severe the injury is.
Neuroimaging the standard goal is determined by computed axial tomography of the skull, which will allow us to evidence the presence of subdural hematoma and the evolutionary phase in which it is (acute, subacute and chronic) and based on the finding determine the surgical therapy or not.
General measures during the admission of the patient to the polytrauma unit, channel via peripheral, parenteral hydration, anticonvulsants if the patient has presented convulsive pictures, suture and clean wounds that generate significant blood loss and worsen or generate hemodynamic alteration (correct hypotension with fluids to maintain a PAS greater than 90mmHg).

Immediate evaluation by the neurosurgery service, who based on the patient's clinical and tomographic findings will determine the behavior, either conservative or emergency surgical.
Compilations after the Surgical act:Post-operative infection, which is usually serious, as it involves the CNS and meninges.
Re-bleeding or formation of new hemorrhages. More frequent in patients with hematological alterations of the Coagulopathy type.
Recurrence of Subdural Hematoma.
Male patient of 60 years of age, without known pathological antecedents, who initiates clinical picture after rolling, where he receives a frontal contusion, evidencing loss of consciousness not quantified and otorragia, so valued and admitted to a specialized medical center.
Neuroimaging studies were performed, where no significant lesions were evidenced, who at that time only receives treatment with antibiotic therapy at meningeal dose due to the presence of otorrhagia and a small fissure in the cliff of temporal bone, as well as fixed analgesia, epamin, and Nimotop (Nimodipino) with partial improvement.
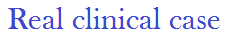
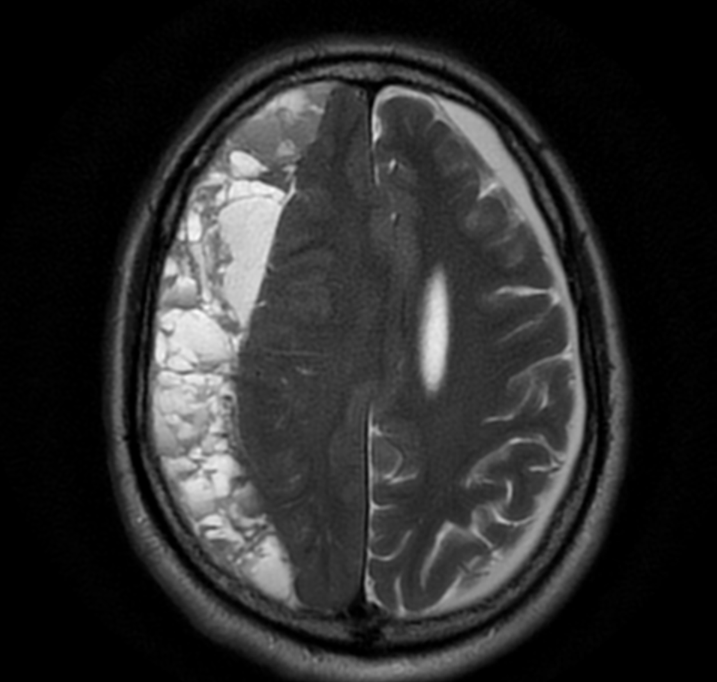
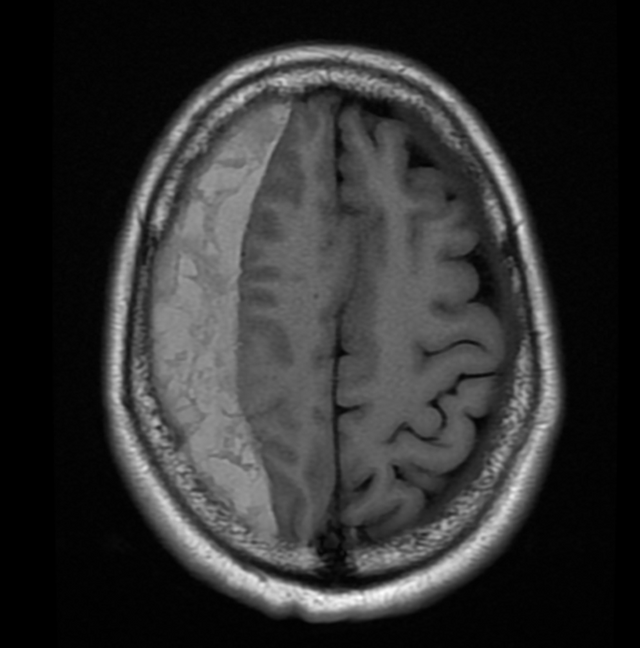
It is associated 5 months after the progressive left hemiparesis event with sudden onset dysarthria and therefore neuroimaging control study is requested, showing the following:

Sagittal T1 @anaestrada12
T2 @anaestrada12
T1 Axial @anaestrada12
Coronal T2 @anaestrada12
At extraxial level with extension from frontal lobe to occipital lobe is observed important collection. Hyperintense in T1 and T2 that does not restrict in Diffusion that conditions compression and displacement of the structure and of the middle line.
Likewise, there is a collection of similar characteristics, but of smaller size that adapts laminar shape that extends to the parieto-occipital region of hypointense behavior in T1 and hyperintense in T2.
Evidence of right front-temporal subdural hematoma - right parieto-occipital in late subacute stage.
Chronic ischemic demyelinating disease of small vessels. Grade II.
Subfacial hernia.
Left mastoiditis.
In view of the patient's clinical history, traumatic history and finding of neuroimage, it is taken to the operating table where craniotomy is performed, which consists of making 2 holes in the skull, distant from each other, coinciding with the hematoma cavity, where the dura mater and the possible membrane of the Subdural Hematoma are opened, allowing the hematic fluid to escape under pressure. Afterwards, it is washed abundantly with saline serum (to reduce the protein content of the cavity). The operation is finished leaving drains for several days.
Receiving broad-spectrum antibiotic therapy at meningeal doses, anticomtials and subsequent neuroimaging controls, with improvement of the clinical and neurological state of the patient until now.

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
I hope you enjoyed my content.
@tipu curate 2
Upvoted 👌 (Mana: 0/15)
Thank you very much for support
This post is manually curated by @dblog.supporter.
Visit https://dblog.io now! This is a tribe for all bloggers on Steem blockchain.
Thank you :)
Our brains are fragile things! I have some hours logged in the polytrauma clinic. Helped a lot with my balance after initial TBI
Posted using Partiko iOS
We must take care of them :) greetings thank you for reading my post