How to perform dislocation reduction of the temporomandibular joint
In this opportunity I will talk about a very important topic in the health area. In most cases in the area of shock trauma, or polytrauma, are often atypical injuries, but that every doctor during the exercise of his career should know and know how to handle.
We should start by mentioning that dislocation of the jaw or temporomandibular joint (TMJ), usually originates, when there are previous musculoskeletal problems in the jaw, such as joint laxity, congenital hypermobility syndrome or neuromuscular problems (dystonic reactions) that pull the jaw out of the joint spontaneously or by simple and easy movements. They are also the result of direct trauma to the jaw.
In general, every medical specialist must identify this type of dislocation and correct it easily, simply and directly.

Public domain Flickr
Anatomy and physiopathology
The temporomandibular joint has a very particular presentation, since it is composed of two joints separated by a joint disc. The TMJ is located between the temporal bone and the jaw.
It is given the bicondile synovial joint termination, since it is made up of two joints separated by a joint disc, and that these comprise the joint tuber of the joint bone, the fossa and condyle of the jaw. This gives it the property of behaving like a hinge joint and of moving.
This joint together with several muscles, allows us to perform multiple functions such as mastication, opening and closing of the oral cavity, lateral movements, protrusion and retrusion.
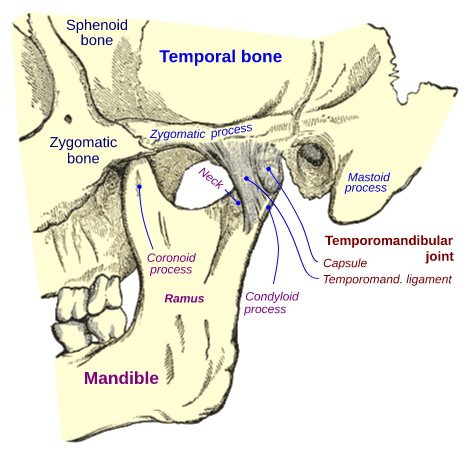
Temporomandibular Joint. Public domainCC BY-SA 3.0
The etiology as already mentioned can be the result of a basic pathology or by traumatic facial injuries, in relation to the first one this can be triggered by simple things like laughing, chewing, during vomiting, yawning, among others.
All of this is due to the fact that during these actions the mandibular condyle can slip in front of the eminent joint of the temporal bone and therefore the anchorage of the jaw muscles pulls the condyle over and forward of the eminent joint causing the jaw to be fixed in a dislocated position and rarely returning to its normal position.
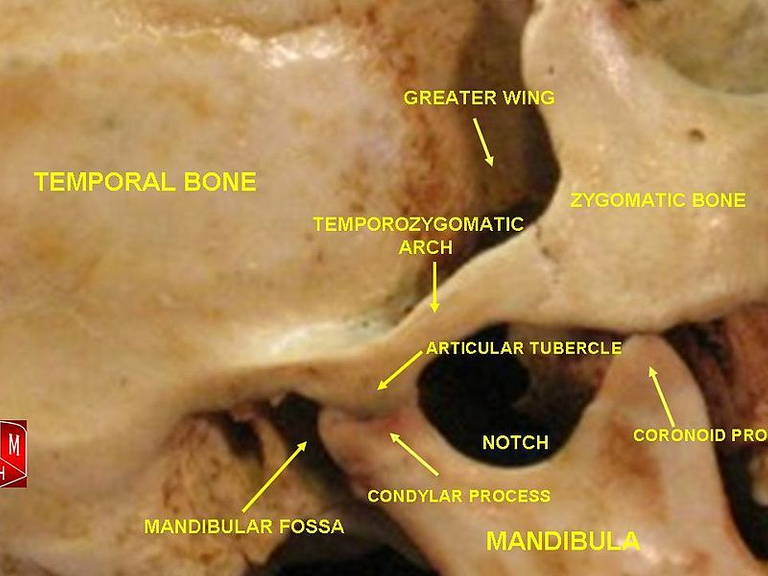
Temporomandibular joint. By Anatomist90Public domain CC BY-SA 3.0
Dislocations can occur in several ways, such as:
Anterior dislocations can manifest themselves spontaneously, in healthy individuals and occasionally return to their normal position.
TMJ dislocations are usually bilateral, but can also occur unilaterally.
Posterior, superior and lateral dislocations are less frequent and are associated with direct trauma to the jaw with or without a jaw fracture.
The diagnosis of these dislocations is simply clinical, and they are corroborated by X-ray studies or more complex studies such as tomography.
Pain is the cardinal symptom in this lesion, and it is presented when executing opening, protrusion and closing movements. A unilateral dislocation causes the jaw to protrude to the non-dislocated side and therefore a palpable depression is observed in the preauricular injured area.
We should try to reduce dislocations of dislocations of jaws that are closed and not accompanied by jaw bone fractures, as long as the patient is conscious, cooperative and under his consent.
When is reduction contraindicated?
All those cases of open dislocations, both superior, posterior and lateral, should be evaluated by surgeons or otolaryngologists.
If it is associated with mandibular bone fractures, they should be evaluated by specialists to determine whether or not reduction will be performed.
When it is associated with nerve endings or lesions of cranial pairs, it is necessary to be urgently evaluated by a specialist before the reduction if possible, or in its defect be taken to the operating room and resolve under general anesthesia.
)
3D mandible fracture. Public domain CC BY 3.0
Initial assessment
Always every physician before performing a simple or complex medical procedure must explain it to the patient and/or his representative and thus obtain the signed consent.
Once the patient is completely examined and we proceed with the reduction, it is advisable to place the patient in a seated position, with a solid headboard, in order to support the head.
It is recommended that prior to the procedure, endovenous analgesia and the use of muscle relaxant type drugs be applied to facilitate the manipulation of this area and to bring the jaw into place in the simplest and least traumatic manner.
The use of these drugs (analgesia or sedation and intravenous muscle relaxants) is essential, especially if the jaw has been dislocated for more than 6 to 8 hours.
There is another alternative as is the case of direct analgesia in the TMJ, we proceed to locate us in the depression resulting from the dislocation about 2.5 cm in front of the ear swallow and just above the condyle (head) of the jaw.
After asepsis and antisepsis of the area, a needle is inserted perpendicularly to the skin and medially up to about 0.5 cm and the anaesthetic solution is administered approximately 1 CC.
How to correctly perform the jaw reduction?
The materials required for this procedure are very simple and straightforward, only requiring a pair of gloves and gauze.
We proceed to place the gloves and wrap several layers of gauze around each thumb, thus preventing any injury to the doctor during the reduction.
Once the patient is in the position already described, the doctor can sit or stand in front of the patient.
Place both thumbs inside the patient's mouth and over the back molars of the jaw bilaterally, place the index, middle, ring and little fingers around the jaw, placing the index fingers behind the jaw angle.
Gentle downward and backward force will be applied to allow the chewing muscles to relax, as the downward pressure releases the mandibular condyle from the articular eminence of the temporal bone.
The patient is asked to open the oral cavity completely, which encourages the impacted mandibular condyle to be released on the anterior articular surface of the TMJ eminence.
This, in conjunction with the procedure described, helps to put the TMJ back into place.
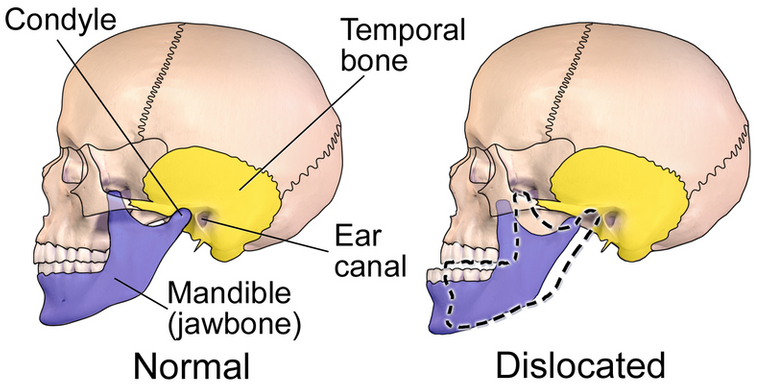
A medical illustration depicting a normal vs. dislocated mandible. Public domain CC BY-SA 4.0
Check if the reduction was done correctly
The patient will be asked to be able to open and close his or her mouth, which will run smoothly and on its own.
It is not necessary to request post-reduction x-rays, unless a fracture is suspected during reduction or a fracture has already been observed prior to reduction, but of little significance that has not contraindicated reduction, and x-ray checks are requested to verify the post-reduction status.
Recommendations
Complications
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.
@tipu curate
Posted using Partiko Android
Upvoted 👌 (Mana: 10/15 - need recharge?)
thanks @ritch
Very interesting !
Posted using Partiko iOS
Thanks :)
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
thank you very much steemstem
Congratulations @anaestrada12!
You raised your level and are now a Minnow!
Vote for @Steemitboard as a witness to get one more award and increased upvotes!
Thank you
TMJ, the one joint u don't wanna mess with I'd you want to keep talking and communicating well with others.
Great write up and highly educative. Steemstem is getting much better each passing day with such content.
Do you mind we converse on discord, would love to ask you a little question.
Thanks
Username is @cyprianj on discord
Hi @cyprianj, thanks for your comment... I'm very happy that my content is to your liking. You can write to me at discord whenever you want