Brain abscess from untreated otitis media
Brain abscesses correspond to the presence or collection of pus within the cerebral parenchyma or in this case in the cerebellum and that will be located by several stages based on its evolution. This pathological entity has its risk factors that predisposes to its appearance as infectious foci near the nervous system that for continuity favor the formation of such absced lesion, such as internal or middle otitis, mastoiditis, facial abscesses, periodontal peri-amigdalino among others.
Practically the germs involved are determined according to the immune status of the patient, and whether the same derived from an adjacent primary focus as in the case of acute otitis media and / or mastoiditis, which is most often associated with a Gram-positive microorganism.
Acute otitis media tends to be observed more frequently in paediatric age, with less incidence in adults, clinics is typical, can take with otalgia, fever and discharge of secretion through the affected ear canal, the idea is these cases is early diagnosis and medical treatment and correct by extending the coverage to germs that are flora of the area itself, with subsequent cultivation of the secretion of the ear if possible.
This publication describes the real clinical case of a 30-year-old woman who, during her last trimester of pregnancy, is associated with symptoms of fever, otalgia with exit of purulent secretion through the right ear canal which then passes from headache, vomiting and meningeal signs, for which she is assessed and admitted.
The objective of this review of the bibliography lies in the importance and medical necessity of attention to pathologies as simple as otitis which, if diagnosed in time, treatment is usually ambulatory and of quick resolution, but when this is not the case, multiple complications arise, such as the feminine one from case to debate, who deals with the symptomatology of neuroinfection, whose infectious focus closest to the central nervous system is the auditory canal.
Anatomy
We begin by remembering that the auditory canal is divided into internal and external, for our study we will bring dimensioning of the internal portion. In a simple way, the external portion is represented by the auricular pavilion and its different structures that characterize it, such as the helix, antihelix, swallow, lobe, shell, cartilaginous portion among others.
The external auditory canal is characterized by a cylindrical canal formed by a fibrocartilaginous portion and another bone, delimited by the tympanic membrane that separates it or determines the boundary between the external canal and the middle.
The middle auditory canal, made up of the petrose portion of the temporal bone, and includes the tympanic cavity represented by the chain of ossicles (hammer, anvil and stirrup), the eustachian tube and annexes of the mastoid.
The internal auditory canal, the portion that houses the auditory sense, made up of the cochlea (contains nerves of hearing), vestibule (receptors of equilibrium), and the semicircular canals.
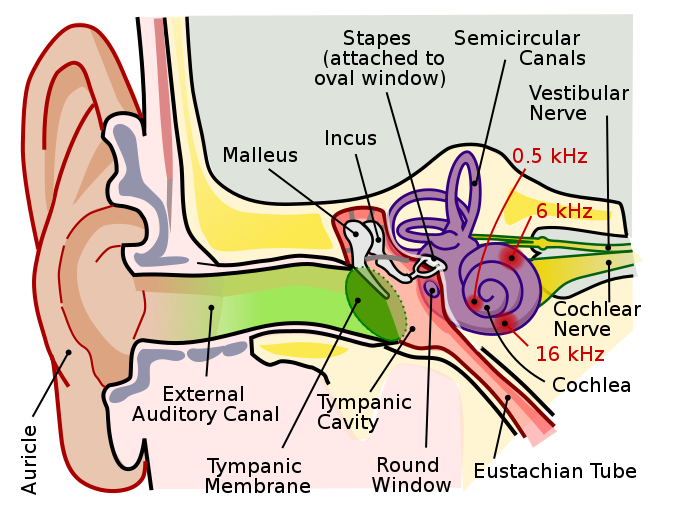
Ear Anatomy. Public domain CC BY-SA 2.5 wikipedia
Cerebellum
It is an essential organ, small and odd size of the central nervous system, located in the posterior cranial fossa below the occipital lobe behind the brainstem. They consist of a large number of nerve fibre bundles whose function is to allow the connection of the cerebellum with the brain and spinal cord.
This anatomical structure is smaller in relation to the brain, is made up of two hemispheres with a center called vermis. This in turn is subdivided into 3 lobes; anterior, posterior and floculonodular. The surface of the cerebellum is constituted by gray substance and in its center in branched form the white substance.
The cerebellum is responsible for integrating the information received from the outside and thus control the orders issued by the cortex to the locomotor system by means of the motorways in addition to this is characterized by being a regulator of physiological tremor. It is for this reason that when there are lesions in the cerebellum there is no hemiparesis (loss of strength) if not alteration in the execution of voluntary movements and alteration in balance and posture.
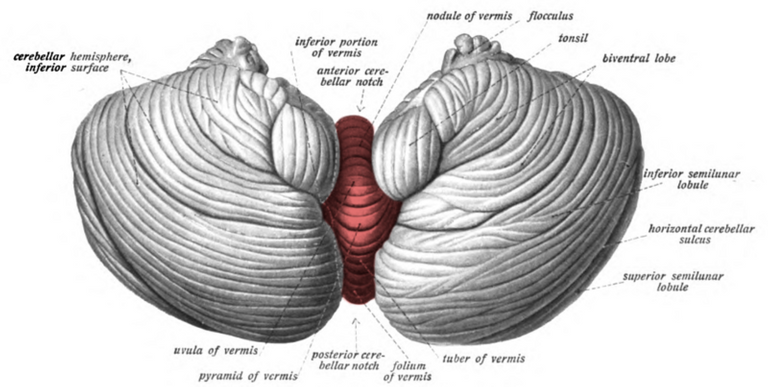
Cerebellar vermis. Public domain CC0 1.0 wikipedia
Brain abscess
As a brain abscess had already been defined, it is described as a collection of pus inside the brain parenchyma, the neurological clinic will be based on the location and size of the lesion.
This pathology was first described in 1893 by the Scottish neurosurgeon William Macewen, who describes 25 cases and which were treated surgically, becoming the pioneer of this pathology.
The epidemiology has changed in the last decade and this is due to the integration of vaccines into the health system, there is a higher incidence rate in males in relation to female sex with a high mortality rate of more than 30% when not diagnosed and treated on time.
Etiology
It is important to take into account the age of the patient, and whether the same initially course with infectious processes close to the central nervous system, as is the case of otitis, mastoiditis, sinusitis, periodontal abscesses, tonsils, or facial. On the other hand, the immune status of the patient plays a fundamental role for the microorganism involved as the causal agent of the abscess, which is why it is divided into:
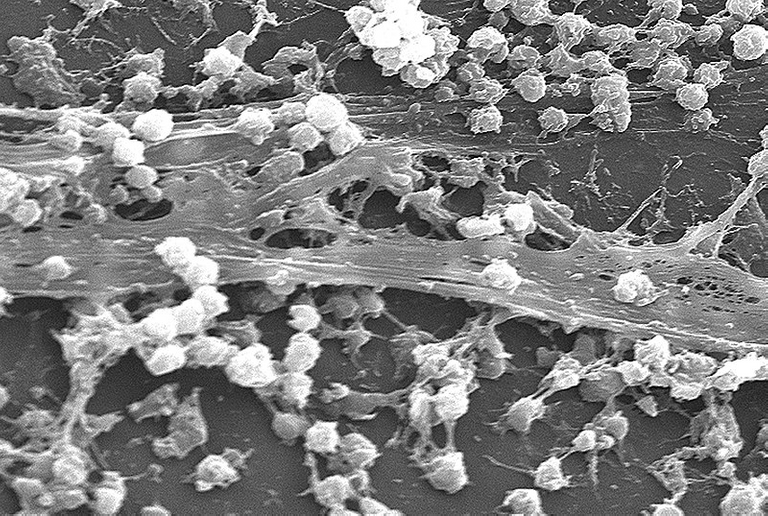
Staphylococcus aureus biofilm. Public domain CC BY-SA 3.0 wikipedia
Physiopathology
Having clear the doors of entry for continuity involved in more than 70%, there are also other pathologies that by hematogenous dissemination are capable of causing brain abscesses such as endocarditis, pneumonia, empyemas, head trauma, placement of catheters or peritoneal valves among others.
Once the microorganism is able to cross the hematoencephalic barrier and reach the central nervous system, it generates a response by releasing cytokines that mediate inflammation (IL8, FNTa, IL1, IL6, MCP1 and BDNF) that alter permeability and trigger quimitaxis.
When the microorganism settles in the cerebral parenchyma, it is preceded by a series of stages:
Clinical Manifestations
It is characterized by a classical triad given by fever, and holocraneous headache of strong intensity and neurological focus.
The neurological clinic will be determined according to the location of the lesion in the nervous system, the number of lesions that can be single or multiple. When the abscess has frontal localization, usually the primary infectious focus starts from frontal sinusitis, the patient may experience agitation, aggression, convulsions and behavioral alterations.
Temporary abscesses may include convulsive crisis, language alteration and quadrantanopsia, while cerebellar abscesses are mostly the product of otitis or mastoiditis, the predominant clinic is ataxia and nystagmus with involvement of cerebellum tests.
Diagnosis
Several methods can be used, however the standard goal continues to be neuroimaging, where an option is the computed tomography of the skull, which will allow us to observe the injury and determine what stage it is and through this study we can monitor the injury with subsequent controls.
The magnetic resonance is the study of choice in the management and diagnosis of brain abscess, much more sensitive than the tomography especially in early stages that offers better resolution and thus determine the presence of the abscess.
The control laboratory examinations are of great help and allow us through them to identify the state of the patient tend to be nonspecific to that during any infectious processes tend to be altered such is the case of complete hematology where we can observe a marked leukocytosis greater than 20,000 cells/ml with a high sedimentation rate, with positive PCR.
The decision of lumbar puncture is not recommended and this is due to the fact that it is an occupant lesion with a mass effect where the cerebrospinal fluid will not be very specific since we can observe hypoglycorrhagia, proteinorrhagia, however in 30% of cases the CSF may be sterile.
Blood cultures with a specificity of 40% but which may be negative and this does not exclude the presence of brain abscess, which is why it is not very useful.
Treatment
The empirical medical treatment that I wish to use must be directed at the pathogen that is suspected to be the causal agent of the abscess, and that said antibiotic scheme correctly penetrates the blood-brain barrier and reaches the lesion.
Initially it is suggested to start with a broad-spectrum triple-spectrum antibiotic therapy based on Vacomycin, Ceftriaxone, and Metronidazole, with good CNS penetration and coverage of polymicrobial germs, which is why it is recommended to start with this triple therapy. As an alternative, ciprofloxacin plus Meropenen or amplicillin sulbactan or Linezolid, especially in these cases of methicillin-resistant staphylococcus aureus resistant to vancomycin.
The treatment with antibiotic therapy must be fully complied with for 28 days with subsequent control of cerebral magnetic resonance.
Steroid therapy (glucocorticoids) especially with those large lesions with mass effect and perilesional edema, is recommended the use of dexamethasone for a short time, as there are studies that have shown that steroids tend to decrease antibiotic penetration to the abscess, increases the risk of rupture of the ventricle and retards the formation of the abscess capsule, however the use of the steroid decreases mortality and the presence associated with symptoms of endocranial hypertension.
The use of anticonvulsants has been necessary in some occasions and this will depend on the location of the lesion as already mentioned. Those lesions with high convulsive power should be treated or if the patient debuts with tonic clonic movements as a cardinal symptom, the use of phenytoin (epamin) 100 mg intravenous or orally is recommended.
Real clinical case
Female of 30 years without base comorbidities, who refers to present since 10 days ago, otalgia and exit of purulent secretion of right ear, accompanied by fever at 39 º C so it goes to doctor who indicates treatment with amoxicillin plus clavulanic acid, which meets irregularly with persistence of picture associated with headache holocraneana of strong intensity, dizziness and vomiting in number of 3 food content with subsequent alteration of the gait so it is valued and entered.
A patient who denies important pathological antecedents, denies smoking habits, winemaking and drug use. Prior to admission, the patient shows otalgia, headache fever, a week of evolution indicates treatment for a suppurative otitis media with amoxicillin plus clavulanic acid and complies irregularly. To the physical examination the positive thing was that it was observed exit of purulent secretion through right ear with flush heat and right peri auricular edema with impossibility of observing the auditory canal, neurologically the patient was conscious, oriented in the three planes, without alteration of cranial pairs, muscular force conserved normoreflexica, positive cerebellar tests, with ataxic mark and rigidity of nape.
In view of clinical picture it is decided to request neuroimaging studies in this case Simple brain magnetic resonance with the following findings:
Hypointense image of approximately 3 cm is observed in cerebellum of irregular edge with edema around the lesion. Right mastoiditis is also evident.
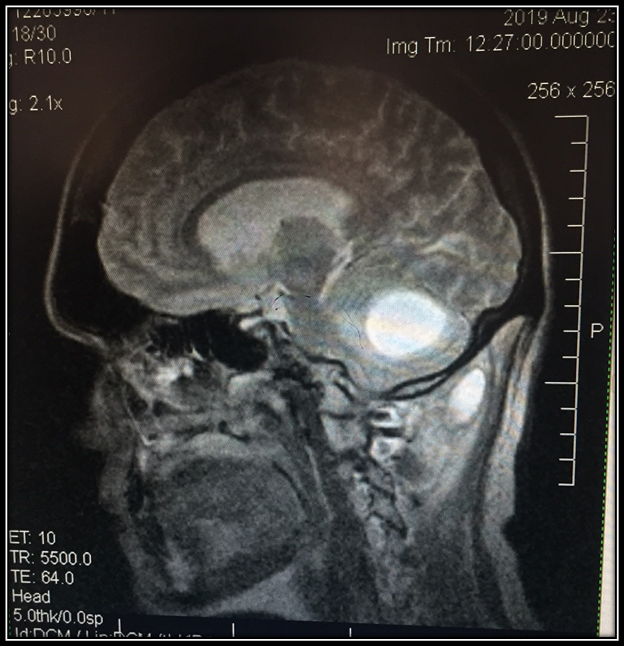
@anaestrada12
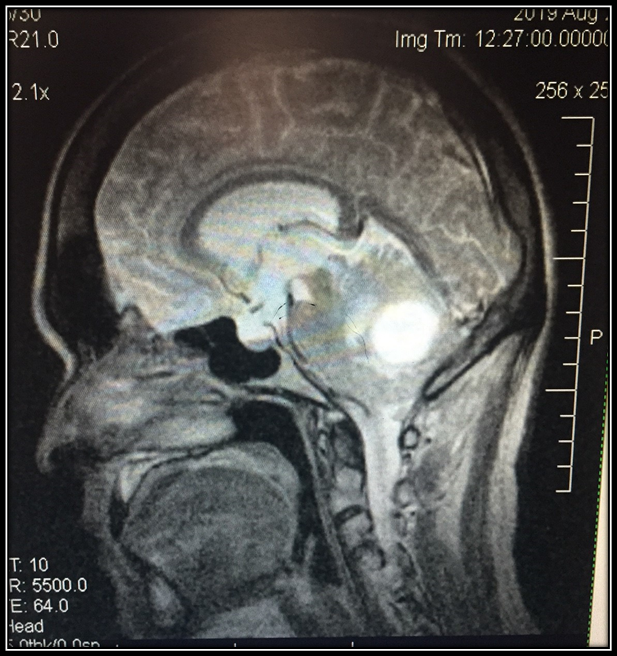
@anaestrada12

@anaestrada12
Patient who is admitted, receives treatment with vancomycin, ceftriaxone and metronidazole for 1 month, with improvement of the clinical picture. Currently without cephalea without neurological alteration waiting to perform cerebral magnetic resonance control.
Sources

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
I hope you enjoyed my content.
Hello,
Your post has been manually curated by a @stem.curate curator.
We are dedicated to supporting great content, like yours on the STEMGeeks tribe.
Please join us on discord.
Thank you very much @stem.curate
Questo post è stato condiviso e votato all'interno del discord del team curatori di discovery-it.
This post was shared and voted inside the discord by the curators team of discovery-it
Thank you @discovery-it
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Thank for support @steemstem
It is kind of surprising to me that the CSF is sterile given the status of the patient. Wouldn't at least be some telling characteristic like decreased glucose? On the other hand, is it Contraindicated to do a LP? Or are there any complications?
Greetings @deholt, the patient of the present case was not able to perform lumbar puncture, in view of the country situation, however, the study of brain abscess falls within the protocol, the frequent thing we observe in this case is hypoglycorrhagia, proteinorrhagia, isolation of some germ in the culture. With respect to the contraindication to this procedure it would be that the patient presents signs and symptoms of endocranial hypertension, prolongation of coagulation times, infected lesions at the LP site, among others. Another thing to keep in mind is that you can have a sterile liquid in those patients who have received antibiotic therapy for several days prior to diagnosis.
Sterile liquid (because ATB usage), infection & endocranial HTN. Got it. Thanks a lot for clarifying that for me!
Have a nice day!
[Repeated]