EXCRETION: Structure and Function Of the Mammalian Kidney.
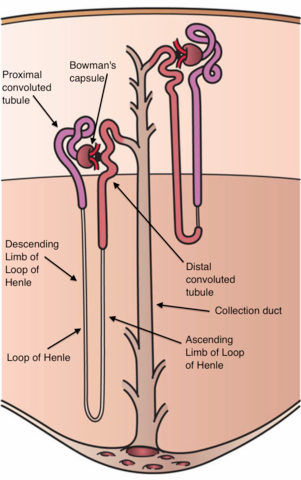
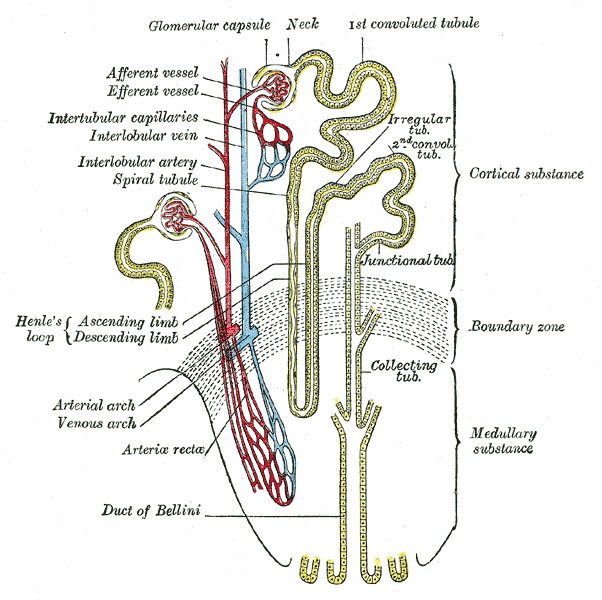
The functional unit of the kidney is the nephron (or kidney tubule). It is important to know the position of the nephrons in relation to the overall plan of the kidney. The outer cortex of the kidney contains the renal capsules (also called Bowman’s capsules) and the first convoluted and second convoluted tubules (also called the proximal and distal tubules), while the medulla houses the loops of Henle and the collecting ducts. Bundles of collecting ducts form pyramids that deliver urine into an open space called the pelvis. From here, urine flows down the ureters to the bladder. Kidney function involves two processes: ultrafiltration and active transport. Ultrafiltration is filtration under pressure: blood is ‘squeezed’ to form a fluid called the glomerular filtrate (usually just the ‘filtrate’). Active transport then modifies the filtrate, secreting some substances into it and reabsorbing others from it, according to the needs of the body. The end result is that blood flows back into the body without much of its harmful waste. This waste, a solution containing urea, salts and various other chemicals, is the urine.
Let’s now look at how individual parts of the kidney contribute to this overall process.
Starting with the nephron: Each human kidney contains about a million nephrons, together with a maze of blood vessels and some connective tissues. There are two different types of nephrons, named after their position: cortical and juxtamedullary. In this section, I will deal with the function of each region of the nephron in sequence, but you must remember that the nephron functions as a whole: the activities of one region are essential to the effectiveness of others.
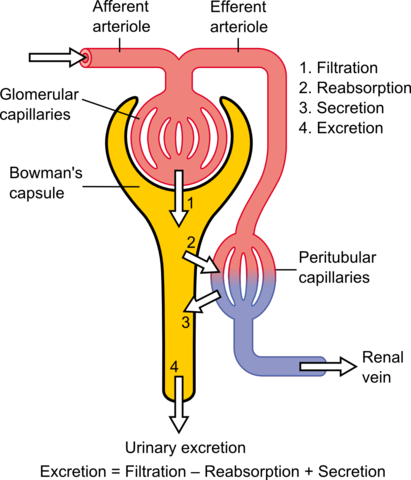
Ultrafiltration in the renal capsule: The renal capsule is shaped rather like a wineglass, with a central knot of blood vessels called the glomerulus. This area of the nephron filters blood by ultrafiltration (filtration under pressure). Obviously, this requires two things: a means of creating pressure and a filter. The kidneys receive blood from the first branch off the aorta, so the blood is already under pressure when it reaches the nephron. This pressure is maintained and enhanced because the afferent arteriole, the blood vessel that takes blood into the glomerulus, is short and has a larger diameter than the longer efferent arteriole that takes blood away. This physical or hydrostatic pressure forces blood against a filter that consists of three layers: the lining or endothelium of the glomerular blood vessels, the basement membrane, and the cells of the renal capsule itself.
The membranes are arranged as follows: the middle basement membrane acts as a fine flter and is therefore mostly responsible for the chemical composition of the filtrate. At this stage the filtrate is identical to tissue fluid. The rate of filtrate production is high: about 125 cm3 per minute. However, we do not produce anything like this volume of urine or we would be constantly using the toilet, and would dehydrate rapidly. On average, we produce about 1 cm3 of urine per minute. The rest, over 99 per filtrate, is reabsorbed. In fact, after the renal capsule, the rest of the nephron is concerned with adjusting the volume and composition of the filtrate. Necessary substances are reabsorbed; toxic compounds and excess solutes and water are removed.
Several forces act on the fluids in the renal capsule, opposing or encouraging the filtration process. The high hydrostatic pressure of blood is the dominant force but it is opposed by the hydrostatic pressure and solute concentration of the filtrate.
The first convoluted tubule: In the first convoluted tubule, also known as the proximal tubule or proximal convoluted tubule, many solutes such as glucose and amino acids are totally reabsorbed into the blood by active transport. Normal urine should not contain glucose. Only when blood glucose becomes very high because of diabetes, for example, does the reabsorption mechanism fail. In addition, this part of the tubule is very close to blood vessels that carry blood away from the glomerulus. Blood in these vessels has a low hydrostatic pressure but a relatively high solute potential due to the plasma protein that remain there because they could not pass through the filter. This allows the blood to reabsorb a large percentage of the water from the first convoluted tubule by osmosis. As you can see that the cells that line the first convoluted tubule show all the classic adaptations to active transport: a large surface area, provided by microvilli, and many mitochondria to provide ATP to power the process.
The loop of Henle: The loop of Henle is a long U-shaped region of the nephron that descend into the medulla and then returns to the cortex. The loop creates a region of high solute concentration (low water potential) in the medulla. The collecting ducts pass through this region, and the osmotic gradient between the inside of the collecting duct and the outside draws water out of the duct by osmosis. Consequently, the urine becomes more and more concentrated (compared with body fluids) as it passes down the duct. So the loop is a vital adaptation that benefits humans and other land-living organisms: it allows us to get rid of waste without losing too much water.
In the outline of how the loop of Henle works, it can be seen that the fluid in the two limbs of the loop flows in opposite directions. We describe this sort of arrangement as a countercurrent system. As the fluid travels up the ascending limb, sodium chloride (NaCl) is transported actively out of the limb into the surrounding area. This causes water to pass out of the descending limb by osmosis. The net result is that the solute concentration at any one level of the loop is slightly lower in the ascending limb than in the descending limb.
The longer the loop, the more chance there is for this mechanism to build up a high sodium chloride concentration. If the loop were only half the length shown, sodium chloride would accumulate to only about 600 units. So the longer the loop, the greater the solute concentration, and the more concentrated is the urine that is eventually produced.
It should therefore be no surprise that animals living in dry desert condition have very long loops of Henle. To accommodate this extra length, the medulla of their kidneys is very thick. There is a general rule: the more need an animal has to conserve water, the thicker the medulla and the more concentrated the urine. The kangaroo rat can produce urine that is 14 times more concentrated than its blood plasma. The kidneys of fish, amphibians and reptiles do not possess loops of Henle. These animals cannot produce urine that is any more concentrated than blood plasma.
The second convoluted tubule: While the first convoluted tubule is reabsorbing most of the filtrate, the second convoluted tubule ‘fine tunes’ the remaining fluid, according to the immediate needs of the body. This tubule plays an important role in the regulation of pH, salt and water balance.
The Role of the Kidney in Homeostasis
The kidney contributes to several vital homeostatic mechanisms. Among the most important are regulation of water content and blood volume. The table below shows a typical water balance sheet for an average person, assuming normal activity and a comfortable external temperature. On average, we get almost two-thirds of our water from drinks and a third from food. We obtain a small but important proportion of water from metabolic reactions, notably cell respiration. Some of the water loss shown in the table below is unavoidable. Metabolic waste must be removed in solution, and so some water loss in urine is inevitable. Similarly, water is always lost from the lungs as we breathe out. A significant amount of water is also lost by diffusion through our skin (this is not the same as sweating). When we sweat, we produce a salty liquid to keep our body temperature constant. On a hot day, or during exercise, we lose more water as sweat. Unless we drink more, our water balance is maintained by producing a smaller quantity of more concentrated urine.
| Water gain | Volume/cm3 | Water loss | Volume/cm3 |
|---|---|---|---|
| Food and drink | 2100 | Through skin | 350 |
| Metabolic water | 200 | Sweat | 100 |
| in breath | 350 | ||
| Urine | 1400 | ||
| Faeces | 100 | ||
| Total | 2300 | Total | 2300 |
Dialysis and kidney machines
Dialysis is a method of separating small molecules from larger ones using a partially permeable membrane. Blood dialysis, or haemodialysis, separates the smaller constituents of plasma, such as urea and solutes, from the larger ones, such as proteins. Blood is taken from the patient, usually from a vein in the forearm, and passed into the machine, where it runs through minute artificial capillaries. These are made from a partially permeable plastic that filters the blood. While blood flows inside the artificial capillaries, a special fluid, the dialysate, flows round the outside in the opposite direction.
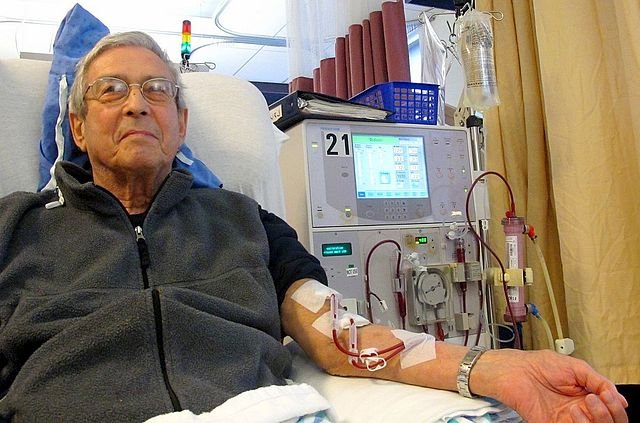
In dialysis, molecules are exchanged between the blood and the dialysate. The composition of the dialysate is carefully controlled so that there is a net movement of urea, water and salts out of the blood. Another type of dialysis is CAPD, which stands for continuous ambulatory peritoneal dialysis. People with kidney failure use one of their own membranes, the peritoneum, as a dialysing membrane. Over 3 000 people in the UK use this technique because of the advantages it offers over conventional dialysis.
The basic principle is simple: the person who needs dialysis has a hole, or stoma, made in their abdomen wall near the navel, through which a large volume of dialysing fiuid is introduced through a tube or catheter. He or she is free to walk around (hence the ambulatory part of the name) while dialysis occurs across the peritoneum between the blood and the dialysate. The dialysate is replaced every six hours by a relatively simple exchange procedure that people can carry out themselves after some basic training.
The mechanism of water balance
Like most homeostatic mechanisms, maintenance of water balance involves a negative feedback loop that consists of a detector and a correction mechanism. A part of the brain, the hypothalamus, contains osmoreceptor that are sensitive to the solute concentration of the blood. When the solute concentration rises, indicating that water loss has exceeded intake, the hypothalamus responds in two ways: It stimulates the thirst centre in the brain, and it stimulates specialised nerve cells in the posterior lobe of the pituitarary gland to release anti-diuretic hormone (ADH). ADH acts on the kidney to reduce the volume of urine produced. It achieves this by increasing the permeability of the second convoluted tubule and the collecting duct to water. The action of ADH causes more water to leave the tubule and re-enter the blood. Much more concentrated urine is produced and vital water is conserved.
Conversely, when fluid intake exceeds loss, the blood becomes more dilute. When the hypothalamus detects this, it reduces ADH production. The action of ADH on the kidneys lessens, resulting in less water reabsorption and the production of larger volumes of dilute, or insipid, urine. People with the disease diabetes insipidus cannot produce ADH because they have a faulty pituitary gland. Once known as the ‘pissing evil’, this condition results in the constant production of dilute urine, leaving the sufferer permanently thirsty and unable to venture very far from the toilet. Today, it can be treated by giving extracted or synthesized ADH.
Finally, on hangovers……!
Sooner or later, most people experience the unpleasant ‘morning after’ feeling which tends to follow a bout of drinking too much alcohol. Many hangover symptoms are due to dehydration, rather than the toxic effects of the alcohol or other ingredients. Research has shown that alcohol inhibits the production of ADH, causing water that the body needs to be lost in the urine. Many of the symptoms disappear when the body is rehydrated. Had people known about the dehydrating effects of alcohol, they could have minimized their headache by having a long drink of water before going to bed (assuming, of course, that he could find the tap in his already drunken state. lol).
Thank you for reading.
REFERENCES
- https://toxtutor.nlm.nih.gov/13-002.html
- https://www.toppr.com/ask/question/what-is-the-function-of-the-kidneys-in-excretion-explain-with-the-help-of-a/
- https://alevelbiologystudent.weebly.com/155-mammalian-kidneys.html
- https://courses.lumenlearning.com/boundless-biology/chapter/human-osmoregulatory-and-excretory-systems/
- http://bio1520.biology.gatech.edu/nutrition-transport-and-homeostasis/animal-ion-and-water-regulation-ii/#:~:text=The%20adrenal%20glands%20sit%20on,lungs%20to%20perform%20this%20function.
- https://www.mayoclinic.org/diseases-conditions/hangovers/symptoms-causes/syc-20373012
- https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/hangovers#:~:text=A%20hangover%20refers%20to%20a,sweating%2C%20and%20increased%20blood%20pressure.
- https://www.davita.com/treatment-services/dialysis/in-center-hemodialysis/how-does-a-dialysis-machine-work
- https://www.healthline.com/health/dialysis#:~:text=Dialysis%20is%20a%20treatment%20that,can't%20do%20their%20job.
I only tried alcohol a couple of times before going teetotaler. We use to jokingly say that the cure to hangover is another couple of bottles of beer. If only we knew then that ordinary water would do it.
Educative piece. Well done.
Thank you for coming by, @gentleshaid.
This last statement, " assuming, of course, that he could find the tap in his already drunken state. lol), really gat me laughing. See what too much alcohol can cause. Very funny.
This is a nice write-up, @loveforlove. Thank you.
Moderation in everything is the best. Thank you for coming, @emperorhassy.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @stemsocial account (for some ROI).
Thanks for using the STEMsocial app, which gives you stronger support. Including @stemsocial as a beneficiary could yield even more support next time.
Upvoted by GITPLAIT!
We have a curation trial on Hive.vote. you can earn a passive income by delegating to @gitplait
We share 80 % of the curation rewards with the delegators.
To delegate, use the links or adjust 10HIVE, 20HIVE, 50HIVE, 100HIVE, 200HIVE, 500HIVE, 1,000HIVE, 10,000HIVE, 100,000HIVE
Join the Community and chat with us on Discord let’s solve problems & build together.