ANIMAL CIRCULATORY SYSTEM: The miracle of open-heart surgery
When the blood vessels supplying the heart muscle become narrowed by fatty deposits, the heart can become starved of oxygen. The patient will suffer pains on exercise – called angina – and is very susceptible to heart attacks. Often, the only effective remedy is surgery.
One of the available operations sometimes known as a ‘cabbage’ (CABG = Coronary artery bypass graft) – takes a team of two or three surgeons about five hours to complete. During the open-heart surgery, the job of the heart and lungs is performed by a heart-lung machine. This sophisticated device also has the ability to lower the core temperature of the body by about 10 C. This reduces the body’s demand for oxygen, giving the surgeons approximately twice as long to perform the operation. The overall aim is to take pieces of vein from the patient’s leg and graft them from the aorta, over the blocked artery and into the heart muscle itself. But how do you sew small blood vessels onto an organ that won’t keep still?
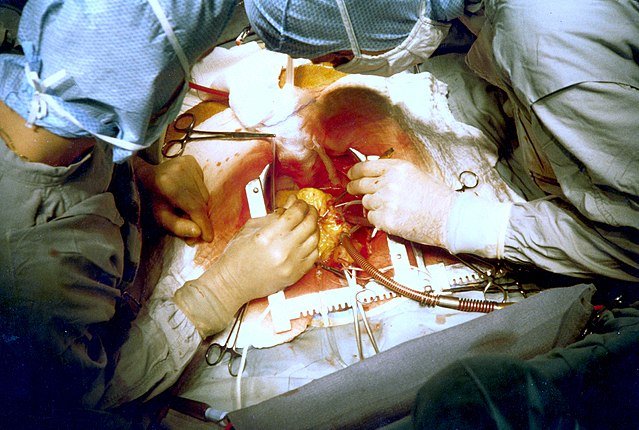
The answer is that you don’t. The heart has to be stopped and this is only possible with a heart-lung machine a device that can take blood from the patient, oxygenate it and return it to the body at the right temperature and pressure. Once this machine has been connected, the heart can be stopped: this is done simply by pouring iced water over it. Once the heart is still the surgeon can sew on the new pieces of blood vessel. When complete, the heart is re-started by means of two electrodes placed on the heart itself.
This standard operation can greatly improve the quality of life for patients, as well as prolonging their life expectancy.
WHY DO ANIMALS NEED A CIRCULATORY SYSTEM?
Evolution has produced large animals, with specialized organs such as intestines, gills and lungs to increase the surface area available for exchange of materials such as food and oxygen. These organs would be relatively useless without a circulatory system, a network of tubes filled with fluid that can deliver vital materials to all the cells of the body, and then take away their waste. In fact, in most animals, almost every cell is within a few micrometres of a branch of the circulatory system.
A circulatory system has three components:
- A fluid that flows in the system, carrying materials around the body;
- A system of tubes that carries the fluid;
- A pump (or pumps) that keeps the fluid moving through the tubes
In vertebrate circulatory systems, blood (the fluid) is driven through arteries, veins and capillaries (the tubes) by the heart (the pump). So, in this post, I will be looking at these three components in detail.
SINGLE AND DOUBLE CIRCULATIONS
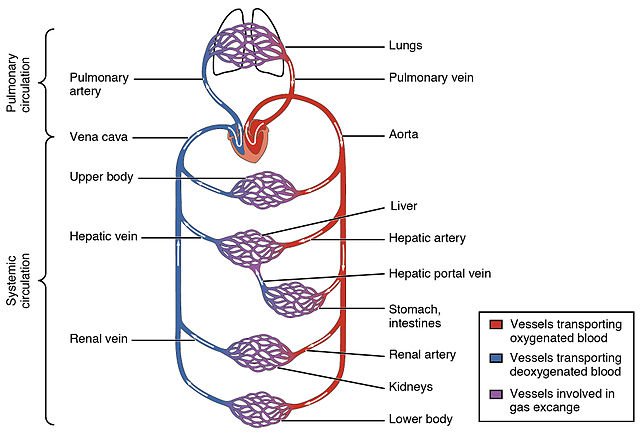
Fish have a single circulation: blood passes from the heart to the gills and then slowly round the body and back to the heart in a single circuit. This system is adequate for fish, but animals with a higher metabolic rate need to deliver oxygen to their tissues faster than a single circulation allows.
Mammals and birds have a double circulation: a pulmonary circulation from the heart to the lungs and a systemic circulation from the heart to the rest of the body. As shown in the figure. A double circulation must have a four-chambered heart. The right side of the heart receives deoxygenated blood from the body and pumps it to the lungs. Here, blood gains oxygen, but loses pressure the left side of the heart receives the oxygenated blood and gives it a boost so that it can reach all the body parts quickly.
THE HUMAN CIRCULATORY SYSTEM
The human heart beats over 100 000 times a day, creating the pressure to force blood through more than 80 000 kilometres (50 000 miles) of arteries, veins and capillaries. The size of the heart is closely related to the organism’s body size. Generally, the heart weighs 0.59 per cent of the total body mass. You can estimate the mass of your own heart using this formula.
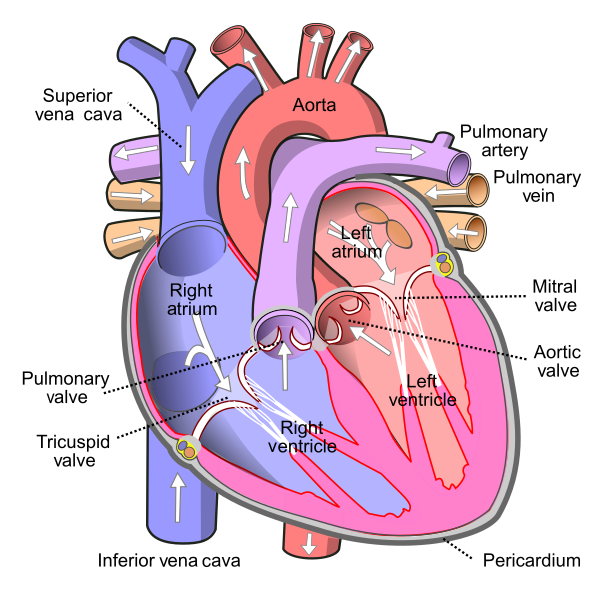
STRUCTURE OF THE HEART
The mammalian heart is composed mainly of cardiac muscle: a specialized tissue that can contract automatically, powerfully and without fatigue throughout the life of the organism. The thickness of the walls reflects their function. The atria are thinly muscled because they pump blood only the short distance to the ventricles directly below them. The right ventricle is more heavily muscled than either of the atria because it has to force blood a much further distance to the lungs. The left ventricle has the thickest wall because it has to force blood all the way around the body. It is important that blood flows through the heart in one direction only. Two sets of valves close to prevent backflow:
- The atrio-ventricular valves (AV valves). These lie between the atria and the ventricles to prevent blood from returning to the atria when the ventricles contract. The tricuspid valve on the right side has three cusps, or flaps. The bicuspid valve, or mitral valve, on the left has two cusps. Both AV valves are subjected to great pressure and ultra-tough tendinous cords are needed to prevent them from turning inside out.
- The semilunar valves guard the openings to the pulmonary artery and the aorta to prevent backflow of blood into the ventricles. Both valves have three semilunar (‘half moon’-shaped) cusps.
HOW THE HEART BEATS
The sequence of events in a single heartbeat is known as the cardiac cycle. The cycle has four overlapping stages:
- Atrial systole. Both atria contract, forcing blood into the ventricles. This stage lasts 0.1 seconds.
- Ventricular systole. Both ventricles contract, forcing blood through the pulmonary artery to the lungs and through the aorta to the rest of the body. This takes 0.3 seconds.
- Atrial diastole. The atria relax, although the ventricles are still contracted. Blood enters the atria from the large veins coming from the body. This takes about 0.7 seconds.
- Ventricular diastole. The ventricles relax, and become ready to fill with blood from the atria as the next cycle begins. This takes about 0.5 seconds. Given an average heart rate of 75 beats per minute, each cycle takes 0.8 seconds.
Valves are simply strong flaps of tissue: they cannot move on their own. A common mistake is to claim that valves can actively control blood flow. For example, the statement: The AV valves close, preventing blood flow, should read ‘blood begins to flow back, forcing the valve shut and preventing any further flow. The heart continues to beat when removed from the body. Individual heart muscle cells grown in culture beat on their own! Because of this, we say that the vertebrate heart is myogenic: the stimulus that drives it to beat originates in the muscle itself. Some invertebrate hearts are neurogenic: they beat only when connected to external nerves.
The electrocardiogram (ECG)
The electrical events that control the cardiac cycle are recorded by placing electrodes on certain parts of the body. A normal, healthy heartbeat produces a distinctive trace. Certain heart defects produce a modified trace and this makes the ECG a useful diagnostic tool.
Features of a normal electrocardiogram (ECG) trace
- R shows contraction of ventricle muscles.
- P wave shows contraction of atrial muscles.
- P-R interval shows time taken for an electrical impulse to travel from sino-atrial node to Purkyne fibres.
- T wave shows relaxation of ventricle muscles.
Control of the cardiac cycle
Heartbeat must be carefully controlled so that each chamber contracts only when full of blood. To achieve this, the events of the cardiac cycle are carefully co-ordinated. A single heartbeat starts with an electrical signal from a region of specialized tissue called the sino-atrial node (SAN), on the wall of the right atrium. This is the ‘pacemaker’, or heartbeat regulator, The electrical signal spreads out over the walls of the atria, causing them to contract
From there, the signal does not pass directly to the ventricles. If it did, the ventricles would begin to contract before they had filled with blood. Instead, the impulse is delayed slightly. A second node, the atrio-ventricular node (AVN) picks up the signal and channels it down the middle of the ventricular septum through a collection of specialised cardiac muscle fibres called the bundle of His. From here, the signal spreads throughout the wall of the ventricles, through the Purkyne (or Purkinje) fibres, and the ventricles contract after they have filled with blood.
Electrical events and volume/pressure changes in the cardiac cycle
We have looked at what happens to the blood that passes through the heart during the cardiac cycle, and at the electrical events that co-ordinate the contraction and relaxation of the atria and ventricles. These events correspond to pressure and volume changes in the heart and blood vessels, and also to the sounds that you hear when you listen to someone’s heart beating.
During atrial systole, the atria fill with blood from the vena cava and the pulmonary vein. Some of the blood that enters the atria flows immediately into the ventricles, without any need for contraction. Atrial systole is initiated when the SAN sends out an electrical signal that spreads out over both atria, causing them to contract and to force the remainder of the blood into the ventricles. There are no heart sounds. Atrial systole is very short, little more than a ‘twitch’. Atrial relaxation, or atrial diastole, lasts for the remainder of the cycle. All the rest of the ‘action’ is in the ventricles.
Ventricular systole begins when the ventricles have filled with blood. The AVN picks up the signal from the SAN and then conducts impulses down through the bundle of His and on through the Purkyne fibres in the walls of the ventricles. This stimulates the ventricles to contract. Blood is forced upwards, forcing the semilunar valves open and the AV valves shut. The closing of the AV valves causes the ‘lub’ of the ‘lub-dup’ heart sound.
Pressure in the arteries rises sharply as blood is forced into them. During ventricular diastole, the ventricle walls relax, arterial pressure walls and blood begins to flow back into the ventricles. This reversal of the flow causes the semilunar valves to shut, causing the second, ‘dup’, heart sound. Meanwhile, the atria have been filling with blood, and as the muscles relax, blood flows from the atria into the ventricles, forcing the AV valves open again.
Stroke volume and cardiac output
The volume of blood pumped by the heart during one cardiac cycle is the stroke volume. A typical stroke volume in an adult is about 80 cm3; every time the heart beats, 80 cm3 of blood is forced through the pulmonary artery to the lungs and 80 cm3 is forced into the aorta to the body. So, the heart pumps over 8500 litres of blood per day. Stroke volume increases during exercise, and regular exercise brings about a permanent resting increase to 110 cm 3, or more.
The volume of blood pumped in one minute is called the cardiac output. It is calculated by multiplying the stroke volume by the heart rate and is expressed in litres of blood per minute.
Cardiac output = stroke volume × heart rate
This is measured in litres per minute and there are 1000 cm3 in a litre.
I will like to stop here for now and continue in my next post where I will discuss how the heart rate can be controlled.
Thank you for reading.
REFERENCES
- Circulatory system
- Transport and homeostasis
- Circulatory system
- Human Body system circulation
- Britannica: Animal circulatory system
- Mammalian heart
- Heart beat
- Heart
- Electrocardiography
- ECG
- Heart regulation
- cardiac cycle
- cardiovascular system/cardiac cycle
- cardiac cycle
- cardiac cycle
- Control of the cardiac cycle
- Stroke volume
Upvoted by GITPLAIT!
We have a curation trial on Hive.vote. you can earn a passive income by delegating to @gitplait
We share 80 % of the curation rewards with the delegators.
To delegate, use the links or adjust 10HIVE, 20HIVE, 50HIVE, 100HIVE, 200HIVE, 500HIVE, 1,000HIVE, 10,000HIVE, 100,000HIVE
Join the Community and chat with us on Discord let’s solve problems & build together.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @stemsocial account (for some ROI).
Thanks for using the STEMsocial app, which gives you stronger support. Including @stemsocial as a beneficiary could yield even more support next time.