An Overview of Testicular Cancer - Cancer of the Testis
Last time, I discussed Bone Tumors, and I explained that there can be malignant and Benign Bone Tumors. Today, I will be pushing further on cancers, and I will be discussing testicular cancer. Before I continue, it is good that we understand what the testicle is very quickly.
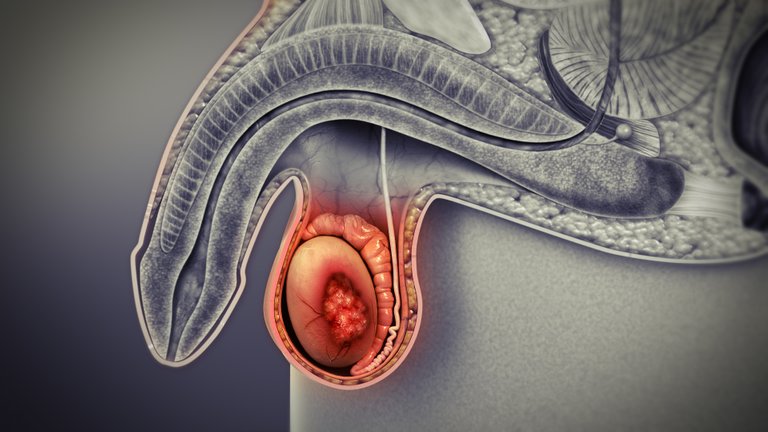
The testicles also known as the testes are located in the scrotum of males. It is about the size of a large Olive and it is suspended in the scrotal sac by the spermatic cord which contains blood vessels, nerves, and the vas deferens. It is responsible for the production of sperm and plays a fundamental role in the production of the Testosterone hormone.
Testicular cancer as the name implies is cancer that affects the testicles. It is one of the most common types of solid cancer that occurs in males between the age of 15 and 35 years. In 2017, there were 8850 new cases and 410 death in the United States. Testicular cancer includes several types of cancer, but I will follow the 2016 WHO updated histopathological classification of testicular cancer.
image
Testicular Cancer can be classified into three major types with other subtypes. These classifications include Germ Cell Tumors, Non-Germ Cell Tumors, and Secondary Tumors.
Germ Cell tumors are a type of cancer that affects the germ cells that produce sperm in the testicles. These cancers include Seminoma, Embryonal Carcinoma, Teratoma, Choriocarcinoma, Yolk Sac Tumor, and Mixed germ cell tumors. Let me take it one after the other. I will not be touching cancers such as Trophoblastic tumors in full.
Seminoma
Seminoma is a malignant germ cell tumor, having a clear or watery cytoplasm with a central nucleus. It is the most common testicular tumor which is common in people between the age of 15 to 40 years. There are three pathologic categories of Seminoma which includes; classical, spermatocytic, and seminoma with syncytiocytotrophoblastic cells. Risk factors for Seminoma include; exposure to chemical compounds like organochlorines, and polychlorinated biphenyls, patients with past history of infections such as mumps viral infection, genetics and family history, trauma, maternal estrogen exposure, and smoking.
Diagnosis and Evaluation include; Scrotal/testicular ultrasonography, laboratory tests such as Serum tumor marker levels, and CT scan of the abdomen and pelvis can be done. Treatment for Seminoma includes surgery, a radical orchiectomy, Radiotherapy, bleomycin, etoposide, and cisplatin.
Embryonal Carcinoma
This is a hemorrhagic or Necrotic cancer of the testicle. The tumor growth begins in the embryonic (fetal) tissue. It often develops in young and middle-aged men, common in Caucasian men. Embryonal Carcinoma presents with a unilateral, and painless testicular mass which could in some cases be painful and cause an aching sensation in the lower abdomen. The clinical test shows an increase in serum human chorionic gonadotropin (hCG), alpha-fetoprotein (AFP), and lactate dehydrogenase (LDH). Serum tumor markers are used to monitor for the recurrence of cancer, and removal of tissue for testing (biopsy). Treatment would include radical inguinal orchiectomy, chemotherapy, and retroperitoneal lymph node dissection.
Testicular Teratoma
Testicular Teratoma is a neoplasm testicular that occurs at a median age of 13 months, it is associated with children and young adults. Risk factors of Testicular Teratoma include Cryptorchidism, hypospadias, family history, atrophic testis, low sperm count, Cowden syndrome, and hereditary conditions such as Cowden syndrome.
Diagnosis includes imaging CT-scan, Magnetic resonance imaging (MRI), chest X-ray, and Ultrasound. Treatment of testicular Teratoma depends on the age of the patient, the histology, and the stage of the tumor. Treatment would include orchiectomy, retroperitoneal nodal dissection, and chemotherapy.
Yolk sac Tumors
Yolk Sac Tumor is a rare type of cancer that affects the ovary and the testicles, but may also affect the chest, abdomen, or brain. It is a common malignant germ cell tumor that affects children. Yolk Sac Tumor presents with high Schiller-Duval bodies which are yellowish and mucinous. Its cause is still unknown but studies show that RUNX3 gene hypermethylation and GATA-4 overexpression may be causes. Diagnosis involves physical examination, imaging studies, and blood chemistry. Treatment includes Unilateral salpingo-oophorectomy and Adjuvant multi-agent combination chemotherapy.
Non-Germ Cell Tumors are a type of cancer that originates from cells other than the germ cells. I will be explaining Leydig Cell Tumor and Sertoli Cell Tumor.
Leydig Cell Tumor
Leydig cell tumors are a tumor derived from Leydig cells that resides in the interstitium of the testicles. The tumors are large with round to oval nuclei. It is acidophilic with granular cytoplasm. The cytoplasm of the tumor shows rod-shaped crystals known as crystalloids of Reinke. Evaluation of Leydig cell tumor would include scrotal ultrasound where it shows as an intratesticular mass. Sonograph can be done, and tumor markers such as alpha-fetoprotein (AFP), quantitative beta-human chorionic gonadotropin (beta-HCG), and lactate dehydrogenase (LDH) should be drawn. Treatment would include radical inguinal orchiectomy, and testis-sparing surgery, it responds poorly to chemotherapy or radiation.
Sertoli Cell Tumor
After the Leydig cell tumor, Sertoli Cell Tumor is the second most common type of pure-sex cord. It is usually found in men between the age of Men 15 to 44 years old. Risk factors include cryptorchidism and familial adenomatous polyposis. Patients with Sertoli cell tumor experience testicular discomfort, pain, and enlarging of the unilateral testicular mass. Diagnosis includes evaluating serum markers, and scrotal ultrasound. Treatment of Sertoli Cell Tumor includes Orchiectomy, Retroperitoneal lymph node dissection, but it has a poor response to chemotherapy and radiotherapy
Testicular Lymphoma is a secondary type of cancer that can occur in the testis. it is a type of non-Hodgkin lymphoma (NHL), that is common in old men within the age of 60 years. Risk factors include age, Exposure to chemicals, radiation, and infection. Diagnosis of Testicular Lymphoma is testicular ultrasound, CT scans of the chest, abdomen, and pelvis. Treatment includes Surgery, chemotherapy, Radiation, and chimeric antigen receptor (CAR) T-cell therapy,
Reference
https://www.hopkinsmedicine.org/health/wellness-and-prevention/overview-of-the-male-anatomy
https://www.ncbi.nlm.nih.gov/books/NBK563159/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5732834/
https://www.mayoclinic.org/diseases-conditions/embryonal-tumor/cdc-20367985
https://www.pathologyoutlines.com/topic/testisembryonal.html
https://www.aafp.org/pubs/afp/issues/2018/0215/p261.html
https://www.ncbi.nlm.nih.gov/books/NBK560513/
https://www.ncbi.nlm.nih.gov/books/NBK448137/
https://www.ncbi.nlm.nih.gov/books/NBK567728/
https://www.sciencedirect.com/science/article/pii/S1930043321000522
https://www.pathologyoutlines.com/topic/ovarytumoryolksac.html
https://radiopaedia.org/articles/testicular-teratoma
https://www.ncbi.nlm.nih.gov/books/NBK563163/
https://www.medicalnewstoday.com/articles/testicular-lymphoma#treatment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758504/
https://www.statpearls.com/ArticleLibrary/viewarticle/24237
https://www.ncbi.nlm.nih.gov/books/NBK549800/
https://www.pathologyoutlines.com/topic/testisSertoliNOS.html
Such a terrible disease with lots of surrounding complexities and the fact that, there is no treatment option is actually terrible.
Thanks for a balanced introduction to a sensitive topic. Here is a wine:
!WINE
Congratulations, @irivers You Successfully Shared 0.100 WINEX With @ireti.
You Earned 0.100 WINEX As Curation Reward.
You Utilized 1/1 Successful Calls.
Contact Us : WINEX Token Discord Channel
WINEX Current Market Price : 0.228
Swap Your Hive <=> Swap.Hive With Industry Lowest Fee (0.1%) : Click This Link
Read Latest Updates Or Contact Us
One of the disease I feared most is cancer because I know it is not Curable