Blood group O is not a universal Donor; why?
Earlier before now and even after graduation from university, we were meant to understand that blood group O is a universal donor. As you delve deeper and acquire more knowledge, you get to understand, there are more to some concepts.
No doubt, the above statement regarding blood group O being a universal donor is true but to an extent false. I know the question in your mind right now is, why? First we will briefly look at the structure of these molecules and how they are naturally formed
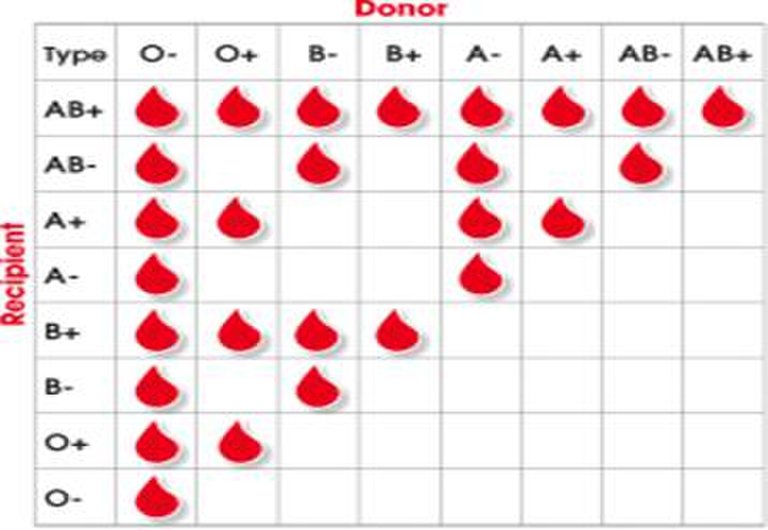
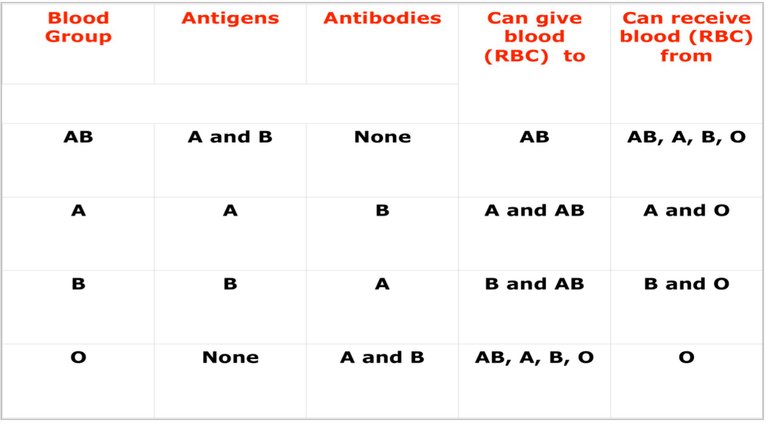
The ABO Blood group system pattern of compatibility
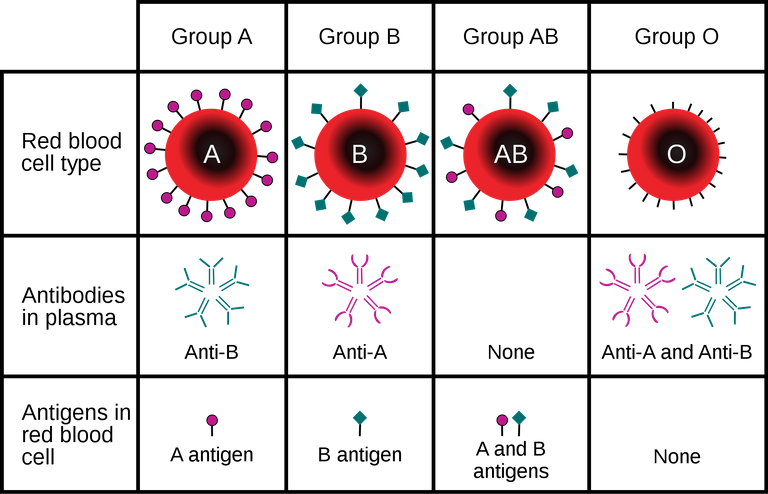
Blood groups (A, B, AB and O) are simply arbitrary terms used to identify or determine the type of proteins or antigens found on the surface of individuals red blood cells. Currently there are about 36 known blood groups but those of clinical significance are the A, b, AB, O and the Rhesus (Rh) blood group system.
These proteins or antigens are mainly responsible for the blood transfusion reactions we hear about. They are located on the cell membrane of all red blood cells. Once they are sensitized at any point, they produce antibodies against the molecule.
Blood group antigens are produced by inheritance of specific genes and it is worth knowing here that – genes produce different antigen options within one blood group system. In essence, there are some genes you must inherit before you can be termed blood group O, A, AB or B.
According to the Landsteiner’s Law when an individual lacks the A or B antigen the corresponding antibody is produced in their serum/plasma.
In essence, if you are blood group A i.e A, it is expected you have the B antibody in your body system. Likewise if you are B blood group, you will have the A antibody in your plasma/serum. If the individual lacks both A and B antigens, then they are referred to as blood group O and they have both the A and B antibody in their plasma or serum.
Individuals that have both A and B antigens are referred to as blood group AB and by implication, they do not produce any antibodies. Understanding and knowing the above principle well gives you a better understanding of why some people cannot receive blood from others and why some can give or receive from other individuals.
In summary, you produce antibodies that are corresponding to the antigens you are lacking.
Reason behind the visible agglutination reactions
Antigens are also referred to as epitopes and on which antibodies bind through their paratopes. The reaction between an antigen and an antibody produces very visible clumping of cells known as agglutination. One major thing I would want you to take home here is that, antigen/antibody reaction producing a visible agglutination is the basis for blood group determination.
Reactions to blood usually occurs when the antigen on the donor cells reacts with an antibody in the patient’s plasma. Like Antigens and antigens do not react nor cause any agglutination reactions. But upon addition of antibodies or antisera, they react.
So whenever you go for blood group testing, what the test aims at is to check any visible agglutination/clumping of cells with one another upon addition of antibodies aka antisera. Agglutination reactions are more visible macroscopically under white background thus, the reason why the test is done on white tiles.
Gene inheritance pattern and Biosynthesis of ABO blood groups
The ABO gene is located on chromosome 9 and has three alleles, A, B and O.
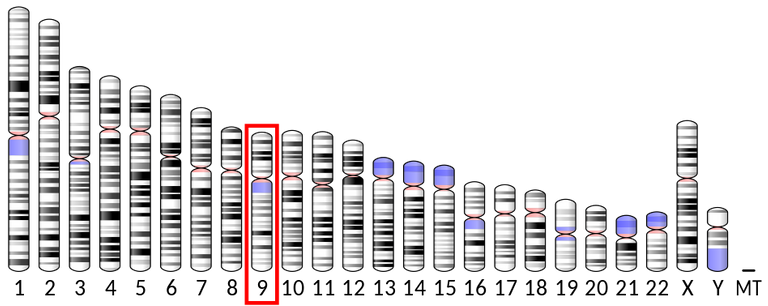
Ideogram of human chromosome with Chromosome 9 highlighted
This alleles (an alternative form of a gene) all encodes differently for specific enzymes known as the glycosyltransferase that adds amino sugars to the precursor H antigen.
Let's briefly talk about the the H antigen.
The genes are the foundation and building blocks upon which all biomelecules are synthesized in the body system. All normal red blood cells have the H antigens on them. This antigen is the major precursor and foundation for other antigens and by implication, you must inherit the FUT1 gene for it to be expressed.
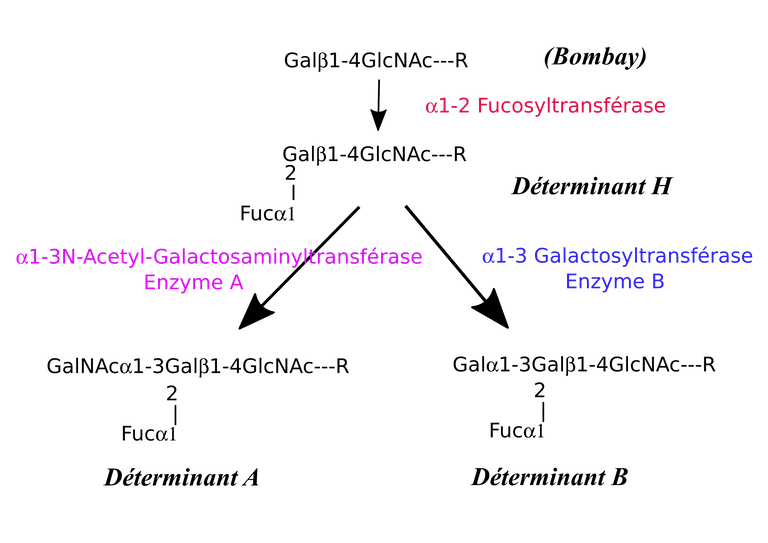
The absence of H antigen in rare conditions is what is referred to as the Bombay blood phenotype (hh).
Bombay (hh)
The Bombay blood group (hh), though rare was first discovered in Bombay by Dr. Y. M. Bhende in 1952. It is mostly found in the India; and its sub-continent, hence the name Bombay.
Since these individuals lack the H antigens, they thus produce anti H antibodies. In essence, Bombay individuals lack the H antigen on their red blood cells, tissues, and secretions, and make they make an anti-H antibodies.
It is worth knowing at this point that, you can only transfuse Bombay individuals with blood from other Bombay individuals. So even blood group O which is to an extent referred as universal donor cannot be used.
Is this the reason why we can't regard blood group O as universal donor? Maybe, maybe not Read on, you will find out soon enough.
Biosynthesis of A, B O blood group
For other blood groups to be formed, the Individual must inherit the corresponding genes that codes for the specific antigens.
A
The A allele encodes a glycosyltransferase enzyme aka 1-3-N-acetylgalatosaminyltransferase that adds N-acetylgalactosamine to the D-galactose end of H antigen. This reaction results to the formation of the blood group A.
B
In a likewise manner, the B allele encodes a different glycosyltransferase enzyme aka 1-3-galactosaminyltransferasethat that adds alpha-d-galactose to the D-galactose end of the H antigen thus, resulting to the formation of B blood group.
AB
In situations where the A and B are co-dominant alleles, i.e you inherit both the A and B alleles, the individual will express both A and B antigens. This means that such individual would be of the blood group AB.
Since they are able to produce both antigens A and B, they do not produce any antibodies. This is one reason why individuals with blood group AB don't have any antibodies in their plasma or serum.
O
The O allele aka (O blood group) is a deletion that results in loss of enzyme translation and therefore presence of unmodified H antigen. So in blood group O, you will only find the H antigen.
The blood group O individual, since they lack both enzymes that catalyzes the enzymatic reaction that adds the sugars to the D-galactose end of the H antigen, they are unable to produce the A and B antigens, thus, they produce antibodies A and B. This is why blood group O individuals have both antibody A and B in their plasma or serum.
The rationale behind blood compatibility testing
Blood can cross react when they are not compatible. Antigens on donor red cells can stimulate a patient to
produce an antibody, if the patient lacks the antigen
themselves.
Just like we earlier pointed out that the basis of the reaction involves the binding of antigens to an antibody, thus producing an agglutination reaction. Recall that individuals produce antibodies to any antigen they lack.
Blood group A (Donor) x blood group A (recipient) since both are of the same blood group, will not react because they contain the same antigens on their cell membrane as well as same antibodies in the plasma/serum.
Blood group A (Donor) x Blood group B (recipient), since they are of different antigens, will react and form clumps. This is simply because, the donor's blood cells contain antigen A, of which the recipient's antibodies can easily bind to, resulting in agglutination reaction. Antigens have antibody binding sites.
Blood group O doesn't have any antigen on its cell membrane, but has both antibody A and B. They can freely donate blood to blood groups, this is why it is erroneously refereed to as the universal donor. This might not be so true once the concept of Rhesus antigen/antibodies and Haemolysin comes into play. Let's take a short dive into the Rhesus blood group system.
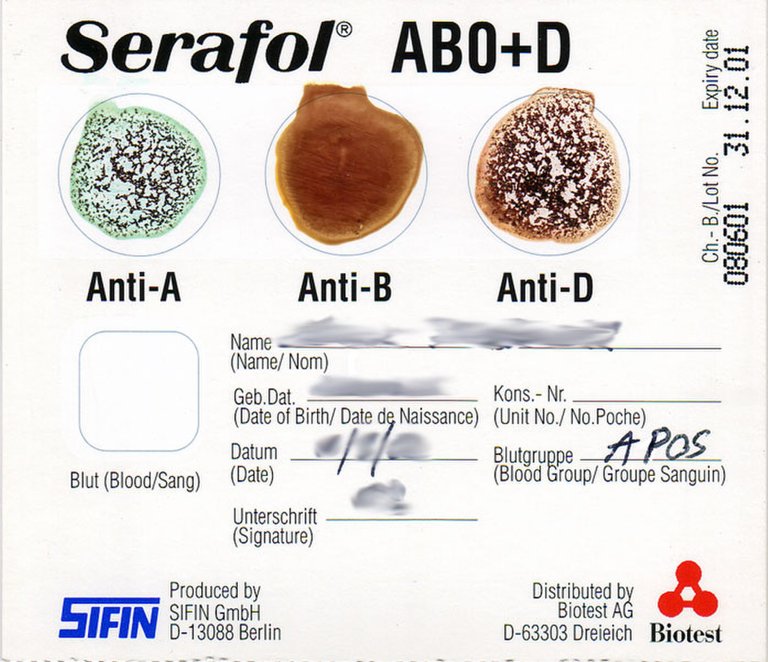
The Rhesus blood group system
The human red blood cells sometimes have another antigen, a protein known as the RhD antigen. When present in the blood of an individual, the person's blood group is referred to as RhD positive. If it's absent, then it is RhD negative.
The main antigen is called Rhesus D. People with D antigen are D positive while those that lack the D antigen are D negative. Now in situations where one who is D negative is exposed to the D antigen, the D negative people produce anti-D antibodies.
The D antigen is also known as Rhesus factor and they are usually arbitrarily attached as +/- to ABO blood group while reporting results. The Rhesus and ABO blood group are the two most important blood group in consideration when it comes to blood compatibility testing.
Rhesus antigens when cross matched with incompatible ones, have the ability of causing sensitization and subsequent agglutination reactions (transfusion reactions). A Rhesus O positive blood cannot be given to a Rhesus O negative person without post transfusion reactions occuring and depending on the strength of the Rh D antibody produced, the reaction could be fatal (especially in the children) severe or mild.
O+ blood contains Rhesus D antigens that are capable of causing agglutination reactions by sensitization of the recipient's blood which produces antibodies against it. The recipient's immune system see it as foreign thereby produces a potent Rh anti-D that causes the agglutination reactions.
As seen in the image below, blood cells of blood group O- individuals to be specific are compatible with patients of all ABO blood groups, be it Rhesus D +/-. In essence, individuals of group O- can be more accurately referred to as universal donors and not just blood group O or O+. In a nutshell, blood group O- is a universal donor instead while AB remains the only universal recipient.
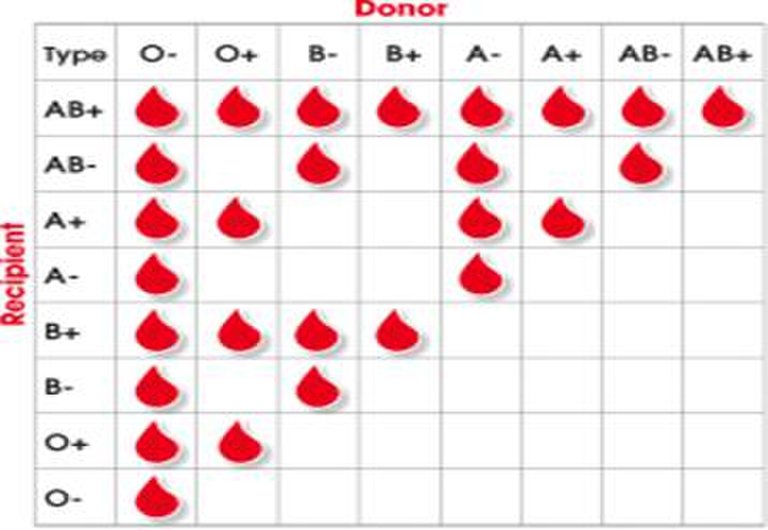
The ABO Blood group system pattern of compatibility
Besides the Rhesus factor, another thing looked out for are antibodies called Haemolysins. Breaking the meaning down - Haemo has to do with blood while lysin is more related to destruction. So haemolysins are antibodies which could be lipids and proteins that cause lysis of red blood cells by disrupting the cell membrane.
Antibodies with haemolytic properties are common within the ABO system. These lytic antibodies are immunoglobulin G (IgG) and in high titres cause haemolysis during blood transfusion.
It is a well established fact that group O donor blood is more readily available and is frequently used as universal red cell donor in many instances. The presence of hemolysins in the donors may however lead to hemolysis in the recipients.
As much as blood group O may seem safe, if it has high concentration of this antibodies, it can lyse or destroy the red blood cells of the recipient. These destruction of red blood cells is usually intravascular (i.e within the blood vessels). Intravascular haemolysis causes the release of the content of red blood cells into the body stream ultimately leading to fever and other associated side effects.
In order to ensure a safe blood transfusion service, they are usually tested for, provided the blood is from a group O donor and the incidence of individual donors having haemolysin in their blood has been reported to be high in such area. The two major ones are the anti-A haemolysin and the Anti-B haemolysin.
Anti-A Hemolysins just as the name implies are able to lyse blood group A recipients blood while anti-B haemolysin lyse the blood group B cells. To be on a safer side, it is better not to give group O donor blood to non group O recipients, if the haemolysin test has not been done to determine its presence in the donors, especially in areas or location that has been reported to have high incidence of people having haemolysin.
Hope you now understand why blood group O or O+ cannot in ideal situation be strictly referred or regarded as universal donors. Only blood group O- has that sole right provided it is is free from haemolysins.
Until I come your way again...
Thanks for reading.
References
•Introduction to haematology and transfusion science
•H Blood Group System
•Biosynthesis of ABO and related antigens
•Haemolysin test for characterization of immune ABO antibodies
•Prevalence of anti-A and anti-B hemolysis among blood group O donors in Lagos
•Blood groups
And then, when you work in blood bank, it’s even more complex than that.
That's very true, it most times only takes expertise to circumvent most challenges that accompanies blood transfusion related issues
Wow I didn’t know about the Bombay blood phenotype. I quickly discussed this with my wife (@lamouthe) and she actually knew about it (she is a nurse). She mentioned that when we account for the fact that people travel a lot hh-people can be found anywhere today.
I have a super naive question. Are there other antigens that play a role, or is the picture you provided the complete one?
Thanks a lot for another great comprehensive blog!
Wao, didn't know your wife is Also on hive ☺️, amazing...
That's very true, diversity also socialization have made it so. Though the incidence of people with the hh is very low.
Regarding the question of possibility of additional antigens playing a role, so far, none to my best of understanding. The ones I discussed here are the major ones. Unless if we decide to delve into the world of Major Histocompatibility complex MHC molecules - antigens that
are looked out for when it comes transplantation of (solid tissues).
I had to put that in bracket because blood is also a tissue but I'm liquid form.
MHC sure will be a topic for some day.
Tanks so much for the lovely contribution ❤️💕
My wife used to be quite active in the past, but has not really any time for it at the moment.
That may possibly be too involved for a layman like me ;)
Lol...maybe
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
You may also include @stemsocial as a beneficiary of the rewards of this post to get a stronger support.
Thanks @cyprianj for this insightful post.
its a pleasure.
thanks for reading.
Congratulations @cyprianj! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s):
Your next target is to reach 25000 upvotes.
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPCheck out the last post from @hivebuzz:
Support the HiveBuzz project. Vote for our proposal!
Interesting read!This explains why patients come down with transfusion reactions even when the donor's blood group is compatible.
Yeah, sometimes, we are just lucky enough that it goes undetected without any problem while sometimes it results to serious post transfusion reactions
This is serious oooo, to think that a large number of us have believed this for years is wierd Sha, but what is life without an increased knowledge, I am glad I came across this post.
We keep learning each day.. there's more to what humans don't actually know.
Another myth busted!
It's the same trouble philosophers get into: they always find exceptions!
Can a regular blood type test uncover such rarities, or will these people have to find out the hard way, if their families don't already know?
Good article.
Nope nope, regular blood test cannot detect them.
They do require special screening
Oh the information overload ;;-;;
Why didn't they teach the rest of the blood types in biochemistry ;;-;;