Bacterial resistance mechanisms
These days I have been reading about bacteria and unusual chemicals. Fortunately these chemicals are rarely used in everyday life, as some of them are lethal. And yesterday I talked very particularly about a bacterium that caught my attention, particularly I did not know it very well, since it is not a common disease, but a question came up in this post and opened me the possibility to develop this topic that I will socialize today with all of you.
Yesterday I talked specifically about the bacetria Bacillus anthracis and the way it has created to generate resistance and tolerance to the most extreme external conditions, which ensures that it can survive for a long time and guarantees to itself the survival of its species. But there are bacteria that generate antibiotic resistance, which represents a major public health problem.
They can avoid antibiotics in different ways, and the reasons for this is usually the misuse of antibiotics. I will share information that I consider important to understand this problem, so I invite you to keep reading, what I am going to tell you will surely interest you.

To understand the mechanisms of bacterial resistance to antibiotics, it is necessary to first understand how antibiotics act on bacteria. The division of antibiotic action is given in two ways:
Bactericidal: these kill the bacteria, usually by damaging the bacterial wall, which is elementary for the bacteria, since it prevents external agents from entering the intracellular space and damaging the DNA or part of its metabolic machinery, necessary for reproduction.
Bacteriostatics: are drugs that do not kill the bacteria, but damage the metabolic systems that allow them to move, grow or reproduce. They prevent the nutrients they need for reproduction and growth from entering the intracellular space. Therefore, over time, as they are unable to nourish themselves, they eventually die. Once they cannot reproduce or grow, the immune system attacks more easily and increases the possibility of eliminating the bacteria.
Basically, these are the two ways in which antibiotics work. Viewed in a general way, of course. The reality is that there are complicated metabolic and cellular processes that occur when the antibiotic comes into contact with the bacteria.
The ideal is, before indicating antibiotics, to perform specific tests such as cultures and antibiograms, to determine which bacteria is causing the infection and to know exactly which is the most appropriate antibiotic.

It usually happens that over time bacteria learn to defend themselves against antibiotics. That is, if one of these drugs blocked an enzyme and prevented the production of proteins necessary for reproduction or growth, the bacteria with prolonged (and insufficient) exposure to the drug, learns and develops a way to prevent protein production from being blocked.
This information of the strategy to defend itself is recorded in the genetic material, which is passed on to the next bacteria that arise from this first one, which will continue perfecting its protection against that particular drug. This generates resistance, which translates into the impossibility for an antibiotic to perform its function on a bacterium or group of bacteria.
This is particularly a public health threat. And people in general do not usually think about this, because they do not see the magnitude of what can be generated if a bacterium emerges that is resistant to all existing antibiotics, it could be something like the declaration of death if you get infected with this super bacteria.
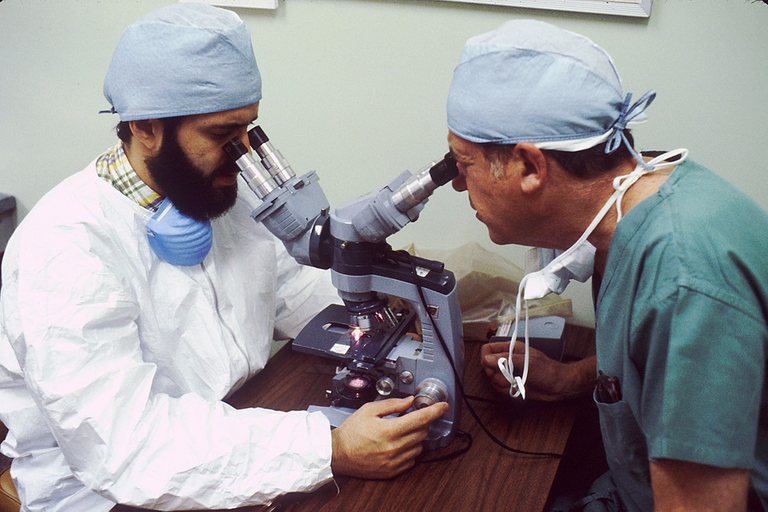
To avoid this problem, from my own experience in a hospital where I worked for a couple of years, they had a bacteriology service that worked closely with the medical staff. This service was in charge of keeping track of the most common bacteria in the hospital and which antibiotic they were most sensitive to.
Not only this, but every three months they performed studies where they *rotated the antibiotics to be used on the same bacteria, to prevent them from developing resistance.
That is, for example, for two or three months they used (in different patients evidently) an antibiotic for a particular bacterium, and then changed the antibiotic to another one. In this way the bacteria were eliminated and were not given the option of developing resistance.
Perhaps they could think about the costs of these studies, but they were simply very little when compared to the lengthening of the hospital stay of patients who had an infection by a multiresistant bacterium. And in this way a very good control of the most common bacteria was maintained, among other data of epidemiological importance.
But this is at the local, intra-hospital level; however, what aggravates the problem is not precisely this, but what happens outside most hospitals.

A common mistake, and one of the main causes of the increase of bacterial resistance, is that in some pharmacies antibiotics are sold without medical prescription, which makes people take them without any kind of care, and evidently, most of the times without even needing them. They take them without any kind of order, they do not comply with the required times, nor with the frequency that is deserved.
This is something difficult to combat, usually hospital services are usually late in terms of care in many cases, so people tend to look for other faster options, and that is when with viral infections the seller of the pharmacy tells you antibiotics. And for a few days, which results in not complying with any protocol for antibiotic use.
There are many reasons why this happens, I just hope that the day does not come when no matter how many antibiotics there are, we cannot stop the bacteria because of the misuse of these drugs.
Did you know about this issue, do you know that this is a big problem that we could face in the future and make it so that there is no curable infection?
There are some bacteria that are healthy for one's life even though it lives in one body
Yes, of course, we have millions of bacteria in our body that fulfill important functions, but in this case I am talking about bacteria that are capable of causing diseases.
You gave me an awesome idea. I think we should talk more about this in hive because the population has some guilty about new types of resistance, right? So the more educated we are maybe we can improve and slow down a bit of new bacterial strains with resistance genes.
!1UP
Of course, educate through hive, reaching more people with this information that surely adds to prevention, through the call for awareness and the proper use of antibiotics.
Thanks for the support.
You have received a 1UP from @gwajnberg!
@stem-curator, @vyb-curator, @pob-curator, @neoxag-curator, @pal-curator
And they will bring !PIZZA 🍕.
Learn more about our delegation service to earn daily rewards. Join the Cartel on Discord.
I gifted $PIZZA slices here:
@curation-cartel(10/20) tipped @apineda (x1)
Learn more at https://hive.pizza!
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.
I usually see this kind of information but act less concerned. Now that I'm seeing it again, a thought just crossed my mind. What if we stopped fighting them ?
Probably divert our research towards making the environment (intercellular space) more symbiotic - we have the power, and everyone gains. They (the bacteria) are actually doing the work they are assigned to. Why would the universe allow their existence in the first place ?