Adenocarcinoma vs Reactive Mesothelial Cells
Just sharing some study slides from cases I previously got to sign out. Cytopathology has been one of the least favorite areas I had exposure. A single slide can take about several minutes to hours just finding a single cell that looks funny.
Most specimens are submitted under the suspicions of malignancy or at least clinicians are trying to rule out malignancy. We get around pleural fluid, ascetic fluid and rarely pericardial fluid as samples. The slides below are just some cases that are common diagnostic problems when calling out whether the cells are malignant or just benign reactions to inflammation.
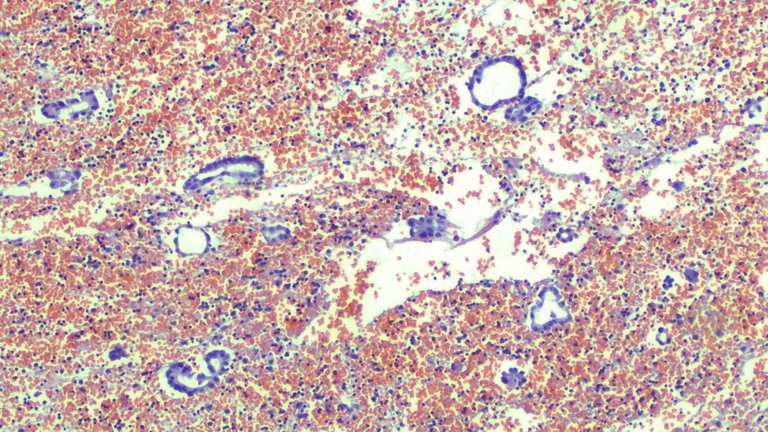
Scanner View
High Power (400x magnification)
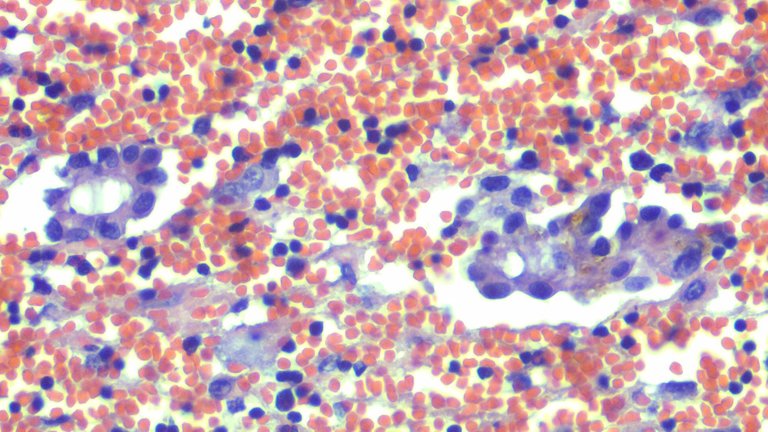
I was confident about calling the specimen out right as positive for malignant cells form this cell block from a pleural fluid sample. See the cells forming something that resembles a gland-like pattern? The clinicians were suspecting a case of lung malignant tumor.
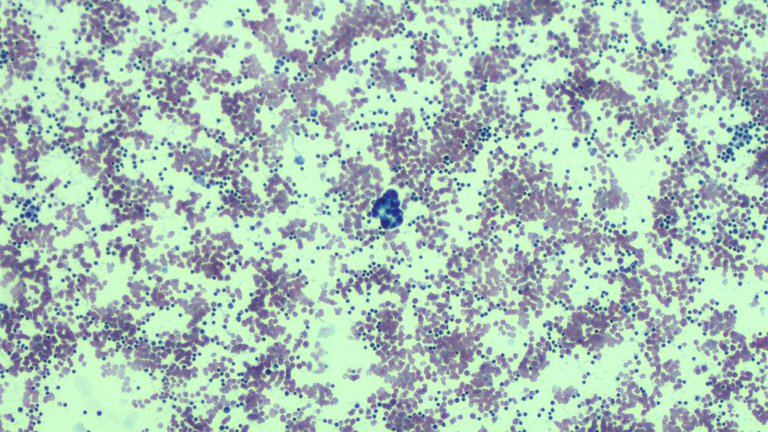
This was what they looked like on smears. Note that cell block and smears are processed differently. Cell blocks are complementary when nothing was found on smears and vice versa.
Scanner View (40x)
High Power View (400x)
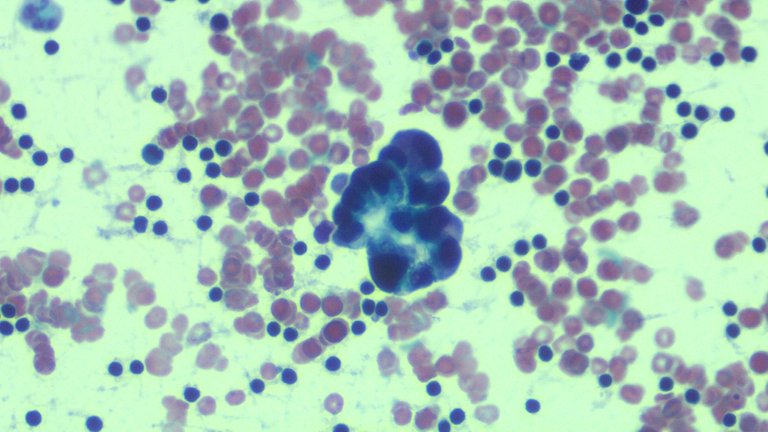
Mesothelial cells would demonstrate some form of windowing where they leave out a small personal space for other cells. If the clusters are arranged in a glandular like pattern, there’s a chance that it’s probably adenocarcinoma but mesothelial cells can also do this too. If there is no lesion on lung imaging, this makes one doubt whether cancer of the lung should really be entertained.
Now confirmation bias is something that is a bitch to deal with. Instead of trying to find ways for you to be wrong, you look at a check list to enforce your calls that this is what it is and you’re never wrong. It was always an understandable mistake to call it instantly an adenocarcinoma or positive for malignant cells as mesothelial cells, when reactive may look like they are malignant.
There are some overt features of malignant cells you can immediately distinguish them from mesothelial cells but when the cellular changes aren’t that dramatic, it’s easy to miss these out. The lesson I learned from the case is exercising more doubt as I was in a hurry to reduce the pile of slides I have to read at the time.
The cells may look like adenocarcinoma but a safer call would be atypical cells suspicious for malignancy. This prompts clinicians to investigate further than immediate being lead to have the patient under aggressive treatment based on your call. The follow up scenario here would be additional stains for the sample or proceeding to surgery (if something in the patient is resectable) to confirm on tissue biopsy.
We do immunohistochemical staining to confirm where the cells being looked at are really mesothelial vs lung cells. That’s for a future post. We don’t do this often to all samples because financial constraints and those stains are pricey to opt for.
If you made it this far reading, thank you for your time.
EDIT: Mesothelial cells are those that line your visceral organs. When I say they are reactive, it means these undergo cellular changes not in their usual state and usually implies a reaction to inflammation. It's important to not be as vague when describing stuff on microscopic findings because words like reactive atypia (implying benign reactions or just not normal but immediately suggestive of malignancy) mean different from plain atypia (implying malignancy or just not normal).
Posted with STEMGeeks
Obviously you have a huge amount of responsibility as what you're doing is making a judgement called based on your knowledge, experience and the following of procedure. How do you deal with the fact that at some point, it's highly likely you'll make a mistake? It's a lot of responsibility to bear, do you ever think about it and how do you cope?
We just do what we can and document it. When unsure, we do pass around the case to solicit some inputs from colleagues and document that it was done. This saves some costs from the patient's part than spending extra to have it looked by another pathologist officially when they can have it done for free while the case is still pending for sign out. Most of the time, it's an out of sight out of mind that once the case has been signed out and benign, 9/10 it won't come back to bite you. The other cases would just be a curve ball to mind and you got to deal with it on a case to case bases.
It's better than having to personally talk to patients and deal with the emotional baggage when making the call. I'm a doctor but I'm not really in touch with the social functions that come with it. I leave that part to clinicians most of the time.
Thanks for that, I love the insights and background as much as the upfront factualities! Really interesting. Best wishes to you :-)
Congratulations @adamada.stem! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s):
Your next target is to reach 3250 upvotes.
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPCheck out the last post from @hivebuzz: