A Case of A Serous Cystadenofibroma
This was from a 67 year-old female that presented with bilateral ovarian new growth (enlarged ovaries). I don’t have the gross pictures here but you’re not missing out on what it looks like live if you refer to this unruptured image, and opened., I don't own those images. These things usually present as ovarian new growths that increase in size over time. Sometimes they'll be an incidental finding on ultrasound because the aren't large enough to cause obstructive or pressure symptoms.
Taken at scanner view 40x magnification
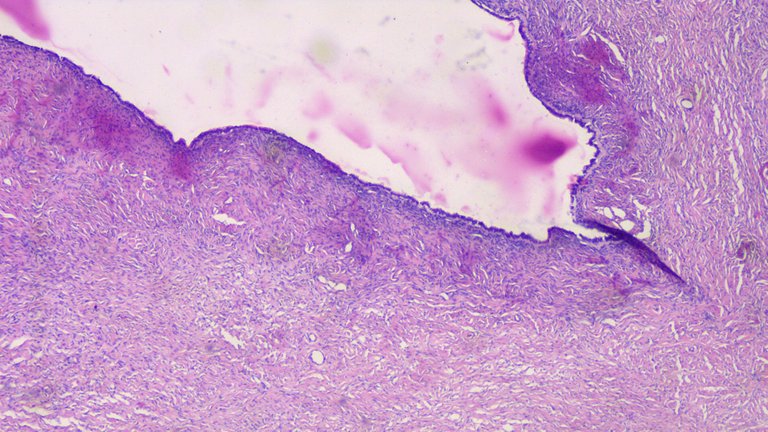
This is the cyst wall, sometimes these can be so thin that you can take the image of an entire wall. Grossly, they can range around less than <0.1cm to >0.6cm thick. You can already see the prominent fibroblastic component on the stroma.
Comparing the stroma between a cystadenoma and cystadenofibroma
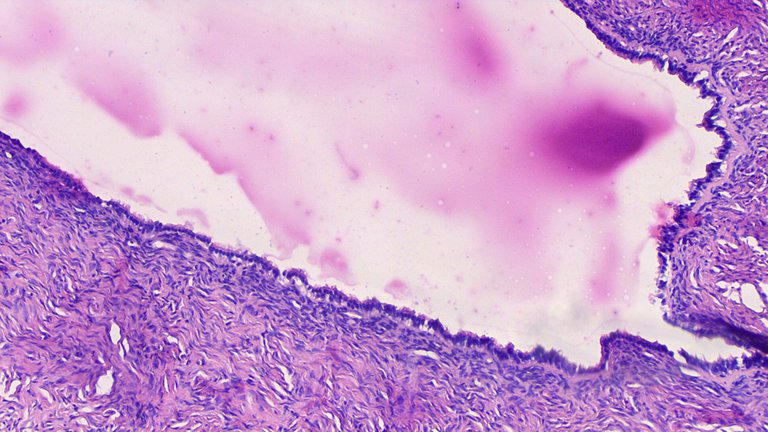
Taken at low power view, 100x magnification.
Taken at high power field, 400x magnification.

This is one of the textbook images to compare it from.
These can be lined by pseudostratified or columnar epithelium. On this case, you can see some tiny tufts of hair like structures on the cells (cilia).
It’s a classic textbook image of what a Serous Cystadenofibroma under microscopic examination. But I still have trouble distinguishing between cystadenoma vs cystadenofibroma where the latter has a prominent stromal fibroblastic component (just the stroma looking more fibrous). This is a small detail and doesn’t affect the prognosis of the patient. It’s one of those situations where you have to encounter them often to get your eyes used to the small details. I get around 1 out of 10 adenofibromas in cases where I thought it’s cystadenoma.
These cases can range for small to large sized ovarian new growth. When grossing this specimen, I look for three things, the type of fluid it contains if it isn’t ruptured, the contents within the walls of the inner cyst especially solid parts, and how many loculations it has.
If the fluid is serous (think of clear to brown water and its consistency), this gives me a lead that I may be dealing with a serous cyst. If the contents look and feel gelatinous (think of semi-solid or gelatin texture), I may be dealing with a mucinous cyst. Mucinous cyst, especially large ones mean I would have to do 2 sections per 1 cm as per recommended guidelines because these can have some areas that may hide malignant transformation. If I suspect a serous cyst, it’s just going to be 1:1 section per cm in size of the tumor.
These maybe hollow or have some focal areas where there are nodule-like thickening. I pick these areas for sectioning because these areas may contain possible malignant transformation. Even if you’re general idea of the case is benign on grossing, if you’re not looking specifically for malignancy, you may miss it, a lot of things can affect your judgment especially if there wasn’t meticulous sampling done. If I happen to section a solid part and then found out that there are skin adnexal structures or organ tissues usually found on other areas of the body, the diagnosis on gross may shift from serous cystadenoma to a mature/immature teratoma.
A cyst may be unilocular or multilocular. Think of an egg with one hollow chamber if you’re dealing with unilocular cyst. Now imagine if you opened the egg but it has multiple compartments which makes it multiloculated. I’m not explaining this in a strict conceptual textbook definition because this is my mental imagery and mnemonics how I remember things so don’t quote me on this. Multiloculations are more associated with malignancy especially when it appears vascular on ultrasound imaging. This just means I need to be more meticulous with sampling.
Some specimens would have a papillary like projections on their lining but nothing like that seen in this case specifically. These type of cases are within the beginner level given how common they are and how easy to process they can be.
If you made it this far reading, thank you for your time.
Posted with STEMGeeks
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
You may also include @stemsocial as a beneficiary of the rewards of this post to get a stronger support.
How many years into your residency now?
!discovery 29
2 years and struggling, 2 more years or 3 if I get some delays on thesis writing. I'm not even sure if I can hold the job given how low my performance is compared to co-residents. Part of the problem is when you are with people that excel at what they do in academics, they can be on steroids in the field.
Being surrounded by them highlights how average my performance is objective but subjectively, yeah I pass the test but the gap is damn high which makes wonder if not being a quitter was the only merit I ever had to be given the position (more than half a year salary-less and I still remained when everyone expects I'd be quitting at the program, imagine just being promised you'll get the position until the official papers were signed kind of moment).
Geez.
Well, persevere it is.
Mabuhay ka adamada!
This post was shared and voted inside the discord by the curators team of discovery-it
Join our community! hive-193212
Discovery-it is also a Witness, vote for us here
Delegate to us for passive income. Check our 80% fee-back Program
Congratulations @adamada.stem! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s):
Your next target is to reach 8000 upvotes.
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPSupport the HiveBuzz project. Vote for our proposal!
I love your descriptions because it is not just work for you, it is passion motivated love! I didn't know that you were still in the residency. I hope they absorb you after finishing it!
!1UP
Click this banner to join "The Cartel" discord server to know more.
You have received a 1UP from @gwajnberg!
@stem-curator, @vyb-curator, @pob-curator, @neoxag-curator, @cent-curator
And they will bring !PIZZA 🍕.
Learn more about our delegation service to earn daily rewards. Join the Cartel on Discord.
PIZZA Holders sent $PIZZA tips in this post's comments:
@curation-cartel(7/20) tipped @adamada.stem (x1)
Learn more at https://hive.pizza.