The First COVID-19 Comprehensive Immunological Model
On April 24, 2020, the first comprehensive scientific model on SARS CoV-2 was published.
The authors are three Italian researchers: Paolo Matricardi, Roberto Dal Negro and Roberto Nisini.
The article is a preprint, very well done, and collects numerous information regarding:
- the onset of the disease
- the method of contagion
- types of acute phase
- immune response
- therapies used so far
In this post I will make a summary of their study, trying to simplify the understanding of some concepts as much as possible, but leaving the common thread of the original article, unchanged so as not to distort the details of the more technical aspects.
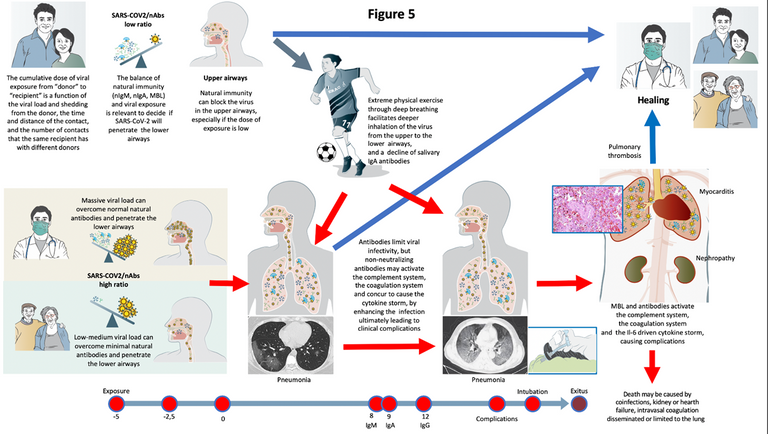
Image CC BY 4.0
The natural progression of COVID-19 (understood as advancing the disease without pharmacological treatment) is extremely variable.
Just as it can occur in the form of an asymptomatic infection, it can develop into pneumonia, leading to various complications that can prove fatal.
While many infected individuals remain asymptomatic or develop only mild upper airway symptoms, others develop pneumonia and acute respiratory distress syndrome (ARDS), which require intensive care intubation and can make the patient's general condition very critical.
People become contagious 2-3 days before the onset of symptoms.
Infectivity appears to decrease significantly already 10 days after the onset of symptoms, but the virus can be detected for a median of 20 days, up to over a month.
First Stage of the Disease
Upper respiratory tract infection
Among infected people, those who develop coronavirus disease (i.e. non-asymptomatic) show their first symptoms on average 5 to 6 days after infection with a minimum of 2 and a maximum of 14 days.
The initial symptoms are limited to the upper airways (cough, sore throat) accompanied by fever, fatigue and muscle pain, while other symptoms are rarer. The sense of taste and smell can go away (without nasal congestion), these are not very frequent symptoms, but they are very specific if they occur.
At the onset of the disease, the virus RNA is usually detected through swabs. However, viral loads, although lower, have also been detected in the swabs of asymptomatic people.
Second Stage of the Disease
About 20% of symptomatic patients develop dyspnoea (shortness of breath) and pneumonia, generally 5-13 days pass from the onset of symptoms to shortness of breath.
Third Stage of the Disease
A few days after the onset of dyspnea, patients develop acute respiratory distress syndrome (ARDS) and require intensive or sub-intensive therapy. This rapid course from dyspnea to intensive care is the reason why monitoring and therapies should often be started when the symptoms are still mild. Acute heart and kidney injuries, sepsis and secondary infection are frequent complications.
Immune Response
Among patients who die from COVID-19, death occurs 2-3 weeks after the onset of the disease. Among survivors, the stay in intensive care (ICU) and then in the hospital can last several weeks.
The immunological model proposed by the researchers explains how to determine the outcome, the first 10-15 days following infection are crucial.
The outcome is essentially determined by the balance between the viral load (linked to the cumulative exposure dose) and the effectiveness of the local innate immune response (natural IgA and IgM antibodies, MBL).
The ability to overcome innate response is linked to three factors:
1) The exposure dose
There is probably a minimum dose, under which the infection does not occur, and then increasingly serious symptoms as the exposure increases.
The greatest exposure occurs in places:
a) closed
b) crowded
c) where there are many infected people
d) where people with more severe symptoms are present
It's no coincidence that hospitals and rest homes are the places where the dose tends to be higher and the health care workers are affected more strongly (compared to the population of the same age).
2) The strength of the innate immune response
It depends on:
1) age (young people have a stronger response)
2) previous conditions (hypertension, immune problems, cancer, obesity, etc)
3) environmental factors
Severe physical stress (e.g. competitive activity) reduces the innate immune response (especially the local airway response), as well as smoking and stress.
The immune response is also modulated by gender and specific genetic polymorphisms: they modulate the response but there's no immune DNA, sex or blood group.
Moderate exercise, unlike intense exercise, improves the immune system.
3) Mechanical phenomena
For example, intense exercise and high flow air on incubation days and in the early stages of COVID-19, facilitates direct penetration of the virus into the lower airways and alveoli, without affecting the mucous membranes of the pathways areas covered by neutralizing antibodies.
Consequences in severe cases
If SARS-CoV-2 overcomes innate immunity blockage and spreads from the upper airways to the alveoli in the early stages of infections, it can replicate without developing local resistance, causing pneumonia and releasing large quantities of antigens.
Being a new virus, the adaptive and specific immune response against the virus occurs after 10-14 days. If the virus has overcome innate defense and has had the opportunity to replicate, the adaptive response will be very strong (high affinity IgM and IgG antibodies).
At this point, three different cascades of mediators are activated:
1) complement system, which causes the release of pro-inflammatory, vasoactive and chemoattractants, which in turn increase local inflammation.
And those provoke:
2) Disseminated intravascular coagulation.
3) Cytokine storm.
These three mediators lead to complications that often require intensive care and, in some patients, lead to death.
In the short span of this pandemic, hundreds of thousands of doctors and researchers have tried to understand the complexity of this disease and the different phenomena it triggers.
At the moment there is no single cure, but biomarkers of the different phenomena and drugs (in addition to the possible antivirals) that contrast the different cascades of mediators that can be triggered have been highlighted.
For this reason, often different pharmacological therapies and different mixes are used that must be carefully dosed and monitored during the clinical course.

As always, I thank all of you for reading and I hope you found the post interesting and clear.
I await your observations in the comments section
See you soon
GM
Source
- Matricardi, P.; Dal Negro, R.; Nisini, R. The First, Comprehensive Immunological Model of COVID-19: Implications for Prevention, Diagnosis, and Public Health Measures. Preprints 2020, 2020040436



@tipu curate 2
Upvoted 👌 (Mana: 24/40)
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider supporting our funding proposal, approving our witness (@stem.witness) or delegating to the @steemstem account (for some ROI).
Please consider using the STEMsocial app app and including @steemstem as a beneficiary to get a stronger support.