#11 [MedBlog] – Neoplasia & Cancer [Part 2]: Development of Cancer & Risk Factors
Hello Hivers,
In the last post we dealt with the definition, differentiation & screening of neoplasia.
In the now 2nd episode, we will dive into the developing cancer and mutations. For that we need to talk a bit about the human genetic code, respectively the DNA and so-called tumor suppressor genes & (proto)oncogenes. In addition, the two-hit hypothesis will be presented to you, the hallmarks of cancer and important risk factors. Bear with me!
The DNA
As some of you may remember from school the genetic code of the human body is encrypted in our DNA – a antiparallel double helix that consists of nucleotides.
Those nucleotides are the basic building blocks of the DNA and consist of a base, sugar & phosphate molecule. The bases used in the human DNA are adenine, thymine, guanine and cytosine. The sugar & phosphate strand build the backbone and the exact sequence of the attached bases present the genetic blueprint.
So, the DNA consists of two strands which represent a relative copy of each other – one is the footprint of the other. Each base has a (physiologically unique) corresponding complementary base on the opposite strand, like two puzzle pieces. Adenine pairs up with thymine and guanine with cytosine.
Accordingly, one knows the exact sequence of the complementary strand if one knows the code of the one strand – e.g. we have the sequence “…AATGCCGTAGC…” on one, we have the corresponding sequence of “…TTACGGCATCG…” on the other – two is better than one, right?
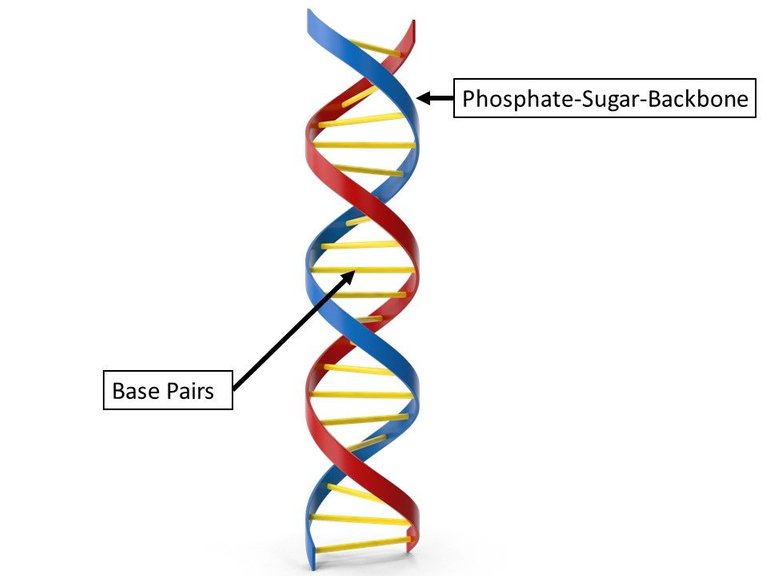
Figure 1: Schematic representation of the human, antiparallel double helical DNA
One base triplet corresponds to one amino acid – several amino acids make up a protein - a lot of proteins make up a cell - a heap of cells ultimately make up the organism.
A gen is simply put a defined section on the DNA that represents the blueprint of a specific protein. Usually a human has 2 alleles of each gen from each parent.
So based on that knowledge, if we have an error in our genetic code, respectively the wrong sequence of bases, can lead to the increased/decreased expression of physiological proteins or with altered functions.
A mutation is simply the alteration of the structure of a gene, resulting in a variant from that may be transmitted to subsequent generations.
Oncogenes & Tumor Suppressor Genes
There are certain genes in DNA that play an important role in the context of cancer development.
Oncogenes are normal genes which regulate proliferation (growth by rapid production of new parts or cells), mobility and differentiation of cells. In the case of a genetic defect that leads to overactivity, for example, this bears the potential for carcinogenesis.
Normally, oncogenes are only active when the corresponding growth factors and signals are present - mutations can decouple the signal path, so that mitotic division of the cell is promoted even without growth factors. Protooncogenes are referred as these genes before mutation. One example would be RAS, a protein that is part in the signal path way of cellular growth – a mutation can lead to an hyperactive form.
| Protooncogene | Neoplasia |
|---|---|
| KRAS | Colorectal Cancer |
| abl-translocation | Chronic Myeloid Leukaemia |
| MYC-amplification | Neuroblastoma |
| HER2/neu | Breast Cancer |
Tumor suppressor genes are also normal genes which inhibit cell division and growth or are part of the DNA repair system. They are often part of the checkpoints in the cell cycle.
A dysfunction here can also lead to unimpeded growth. A famous example is the protein p51 which stops the cell cycle in case of DNA defects.
| Tumor Supressor Genes | Neoplasia |
|---|---|
| RB-Gene | Retinoblastoma |
| APC-Gene | Adenomatous-polyposis-coli |
| BRCA | Breast Cancer |
Protooncogenes and tumor suppressor genes or their respective gene products are opposed as an antagonistic system for controlling the cell cycle and thus tumor growth.
In general, you could say that oncogenes are the result of a dominant, “gain-of-function” mutation and therefore the mutation on one allele is enough to promote cancer growth, while tumor suppressor genes have a recessive, “loss-of-function” characteristic meaning both genes on both alleles need to be affected.
Mutation of the DNA & Repair Mechanisms
Every day approx. 55,000 single strand breaks and 9 double strand breaks occur in every cell of the human body – these are based on both endogenous and exogenous factors. Concerning the mutation insertion, deletion, duplication, amplification, translocations etc. are possible – one more dangerous than the other.
Endogenous causes are mutations, replication errors and radical oxygen species [ROS] (maybe you remember them from Episode #4).
Exogenous causes include oncogenic viruses, physical noxae (e.g. UV light), chemical noxae (aromatic hydrocarbons, nitrosamines, silicates / asbestos, metals and phytotoxins).
For the repair of the DNA damage there are proteins/enzymes of ca. 180 genes available. Following these are the repair mechanisms for single strand lesions:
- Base Excision Repair (BER): with BER - for single strand breaks, oxidized bases, mismatches prior to replication, abasic sites, and deaminated cytosine
- Nucleotide Excision Repair (NER): with TFIIH & XPG – for bulky lesions such as UV-induced thymine dimerization
- Mismatch Repair: with MSH2, PMS2 & MLH1 – for mismatches after replication
For double strand lesions there are two options: - homologous recombination [30 %]: with RAD-51 and usage of the intact region of the homologous strand for faultless repair
- non-homologous end-joining [70 %]: since no homologous template is used, the repair is usually faulty
Two-hit Hypothesis / The Knudson Hypothesis
Tumors arise from the accumulation of mutations, which can be spontaneous, environmental or hereditary causes.
The hypothesis can be clarified, for example, on the basis of retinoblastoma, in which there are hereditary and sporadic forms.
In sporadic retinoblastoma, both healthy alleles have to mutate in one cell in order for a tumor to develop - the likelihood of this is comparatively low.
In the case of hereditary retinoblastoma, one allele is already mutated in the germline, so that in principle every body cell has only one functional, healthy allele - the 1st hit is therefore already in the germline.
As a result, only the mutation of the one, still healthy allele is necessary as a second hit for a retinoblastoma to develop - the likelihood of this is much higher.
Generally speaking, after the 2nd hit, one speaks of the loss of heterozygosity.
Development of Cancer
A 3-stage model is assumed which consists of “initiation”, “promotion” & “progression”.
During initiation, there is a change in the genome due to mutation, e.g. triggered by genotoxic substances.
The tumor promotion leads to a visible tumor resulting out of increased proliferation of the mutated cells. At this stage, the genotoxic substances no longer have to be present, but promoting substances are which serve as a growth signal and are not necessarily genotxic themselves. Examples are e.g. hormones, wound healing factors, alcohol, nicotine, etc.
The final stage so-called tumor progression is defined by a polyclonal tumor cell association that proliferation without external growth stimuli. This is archieved by further mutations & immortalization.
The hallmarks of cancer include:
- permanent growth stimulus
- bypassing apoptosis
- Induction of angiogenesis
- disturbed cell cycle
- immortality
- Invasion and metastasis
- dysregulated energy metabolism
- evading the immune system
- genomic instability & mutations
- carcinogenic inflammation
Checklist
By now ...
✅ you know the structure and components of the DNA
✅ you can differentiate between oncogenes and tumor suppressor genes
✅ you are familiar with damage & repair mechanisms of the DNA
✅ you know the hallmarks of cancer cells
✅ you can explain the development of cancer & the Two-hit hypothesis
Do not forget to follow to not miss out on new content!
See you soon!
Noogie 👨⚕
What's Next?
In the next episode, we'll deal with chronic inflammations as a cause for carcinogenesis and it’s causes!
Congratulations @noogie! You have completed the following achievement on the Hive blockchain and have been rewarded with new badge(s) :
Your next target is to reach 1750 upvotes.
You can view your badges on your board and compare yourself to others in the Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPSupport the HiveBuzz project. Vote for our proposal!
Cancer can be scary as fuck especially in developing countries.
I only had basic oncology classes while in the University. This is s very well detailed and in-depth mini tutorial on the subject. My lecturer then taught us that through dermatoglyphics, medical science can predict possibility of developing cancer in later years, hence such individual will be monitored.
However, learning about the possibility of gene editing, and recognizing the specific genes that causes various cancer, medical science will be able to put an end to the menace of the unhindered proliferation of cells.
Definitely true! - thanks for sharing your experience & knowledge. Targeting cancers at the genome level is definitely the ultimate goal - still a lot of research to be done!
!WINE