This is not an enemy of life!! It is just a condition-Hemoglobinopathies
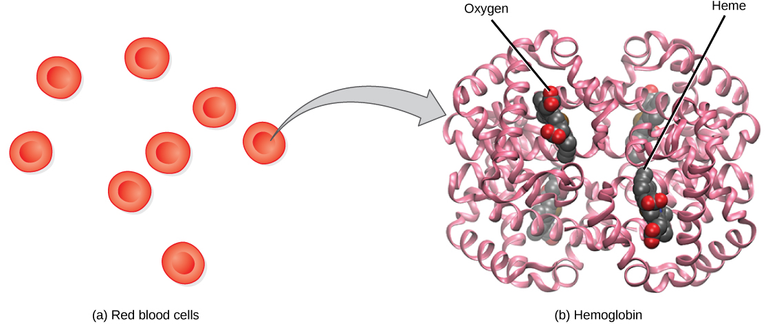
Greetings buddy!! How about starting with a question ❓Have you heard of hemoglobinopathies before? I guess the name doesn't ring a bell to some of us. So, what exactly are hemoglobinopathies? Well, they're simply a group of genetic disorders that affect the structure or production of haemoglobin, which is known as the protein responsible for carrying oxygen in our red blood cells.
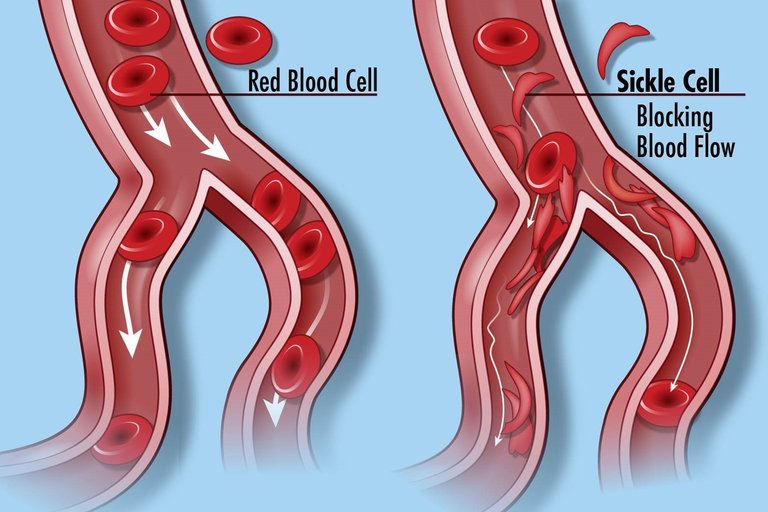
The two most common and recognised types of hemoglobinopathies are sickle cell disease and thalassemia. These conditions, although different in their specifics, both involve abnormalities in the haemoglobin molecules. Sickle cell disease deform the red blood cells to become rigid and sickle-shaped, leading to various complications to the body. I know we all are familiar already with what that means.
Thalassemia, on the other hand, results in the production of fewer healthy red blood cells, causing anaemia and associated symptoms which we are going to see in we move deeper.
Now, I know these conditions might sound complicated to some people, but don't worry, I'll make it simple and engaging! Throughout this article, I'll break it all down for you in a way that it will be easy for you to understand. We'll examine the causes, how they are inherited, the signs and symptoms to look out for, the diagnostic procedures involved, available treatments, and even tips on how to live well with hemoglobinopathies.
So, whether you or someone you know is affected by these conditions or you're simply interested in learning more, this article will provide you with helpful information every step of the way.
So are you ready to journey with me? Let us get started
Here we go!! Now hear the full gist!
We've covered the basics of hemoglobinopathies in the previous section, and now it's time to delve into the causes and inheritance patterns of these conditions. Understanding how they occur can shed light on why certain individuals may be at a higher risk.
Hemoglobinopathies are primarily inherited, meaning they are passed down from parents to their children through genes. The genes responsible for producing hemoglobin can carry mutations, which result due to abnormal formation of protei. These mutations can be present in one or both copies of the gene, leading to different types and severity of hemoglobinopathies.
Sickle cell disease is caused by a mutation in the gene that codes for the beta-globin subunit of hemoglobin, known as HBB. This mutation causes the red blood cells to change shape under certain conditions which I won't be able to discuss in this article, affecting their ability to carry oxygen efficiently while being transported around the body.
Thalassemia, on the other hand, is caused by mutations in the genes that produce either the alpha-globin or beta-globin subunits of hemoglobin. These mutations can result in reduced or absent production of these subunits, leading to low levels of normal hemoglobin and, consequently, anemia.
The inheritance patterns of hemoglobinopathies depend on whether they are caused by mutations in the HBB gene (sickle cell disease) or the genes that produce alpha-globin or beta-globin (thalassemia). Sickle cell disease follows an autosomal recessive pattern, meaning that individuals must inherit two copies of the abnormal gene (one from each parent) to develop the disease. Thalassemia also follows autosomal recessive inheritance but can vary in the severity of the condition depending on the specific mutations involved.
But keep in mind that people without a family history of hemoglobinopathies can still carry the abnormal genes. This is known as being a carrier or having the trait. Carriers typically do not experience any symptoms or health problems related to the condition but can pass the gene mutations on to their children. Genetic counseling and testing are valuable tools in determining an individual's carrier status and understanding the risks involved.
I believe we have now understood better what hemoglobinopathies are. So In our next section, we'll explore the signs and symptoms that can manifest in individuals affected by hemoglobinopathies. Understanding these symptoms will us to detect and carry out effective management where necessary. So stay tuned, and let's explore more together!
Let's move on to discussing the signs and symptoms that individuals affected by hemoglobinopathies may experience.
In both sickle cell disease and thalassemia, one of the hallmark symptoms is anemia. In a nutshell, anemia occurs when the body doesn't have enough healthy red blood cells to carry sufficient oxygen to tissues and organs of the body. This can lead to fatigue, weakness, and shortness of breath, especially during physical exertion.
Another common symptom of hemoglobinopathies is pain. But how? In sickle cell disease, the abnormal-shaped red blood cells can obstruct blood flow, leading to tissue ischemia, or lack of oxygen supply. This, in turn, can result in episodes of severe pain called sickle cell crises. The pain can occur anywhere in the body but is often experienced in the bones, joints, abdomen, or chest. Thalassemia patients may also experience bone pain due to abnormal bone growth and expansion caused by increased red blood cell production in response to chronic anemia.
Due to chronic anemia, individuals with hemoglobinopathies may exhibit pallor, characterized by a paleness of the skin, mucous membranes, and nails. Their bodies may physiologically attempt to compensate for the reduced oxygen-carrying capacity of the blood by increasing heart rate and cardiac output. Consequently, they may have noticeable heart palpitations or a rapid pulse.
Other symptoms can be jaundice, which results from the breakdown of red blood cells by the spleen and gives a yellowish colour to the skin and eyes. Enlargement of the spleen, an important organ involved in filtering the blood, may also occur as the spleen works harder to remove abnormal red blood cells.
Do not forget that the severity and frequency of symptoms can vary widely among individuals with hemoglobinopathies, even within the same condition. Some may have milder forms of the disease and experience few symptoms, while others may require regular medical management and intervention.
Early diagnosis through newborn screening or genetic testing is all we have to do in order to identify hemoglobinopathies and allow prompt management and treatment. This treatment will aims to alleviate symptoms, prevent complications, and improve quality of life. It may include blood transfusions, medication, pain management, and specialized care tailored to the individual's specific needs.
We now move on to the next section, where we'll explore the potential complications associated with hemoglobinopathies and the preventive measures that can be taken. Do you wish to understand better? Then stay with me till the end!!
Complications can arise in individuals with hemoglobinopathies, especially if the condition is not effectively managed. Some of the potential complications include:
Infection: People with hemoglobinopathies, particularly those who have undergone splenectomy, what is called surgical removal of the spleen, may have an increased risk of infection. The spleen as I mentioned earlier plays a crucial role in filtering out bacteria and certain types of pathogens from the bloodstream. If you don't have a fully functioning spleen, then you are more susceptible to infections, particularly from encapsulated bacteria like Streptococcus pneumoniae. Vaccinations and preventive antibiotic therapy are often recommended to reduce the risk of infections.
Acute Chest Syndrome (ACS): ACS is a common and serious complication cause by sickle cell disease. It occurs when sickle-shaped red blood cells obstruct blood vessels in the lungs, leading to decreased oxygen supply and inflammation to tissus. ACS can result in severe chest pain, respiratory distress, fever, and cough. Prompt medical attention is crucial as ACS can be life-threatening and require hospitalization.
Organ damage: Chronic anemia and compromised blood flow in individuals with hemoglobinopathies can cause organ damage over time, this is so common . Organs commonly affected include the kidneys, liver, heart, and eyes. Regular monitoring and appropriate management can help minimize the risk and progression of organ damage.
To prevent complications and improve the quality of life for individuals with hemoglobinopathies, a multidisciplinary approach to care can not be over emphasized. This may involve the collaboration of hematologists, pediatricians, genetic counselors, pain management specialists, and other healthcare professionals, very important . Regular check-ups, comprehensive healthcare plans, and patient education are crucial components of managing these conditions effectively.
As human beings, we need to recognize the psychosocial impact that hemoglobinopathies can have on individuals and their families. Support groups, counseling services, and community resources should provide emotional support, education, and empowerment for those affected by these conditions.
Remember, early diagnosis, proper management, and a supportive environment can significantly improve the quality of life for people living with hemoglobinopathies. Through continued research, education, and medical advancements, we hope towards a future where these conditions are better understood and effectively treated.
If you suspect that you or a loved one may be affected by a hemoglobinopathy, please kindly consult a healthcare professional for accurate diagnosis and guidance on the appropriate next steps.
Thanks for your time and have a nice weekend. I will really appreciate your comments and questions if there's any
References
- https://medlineplus.gov/ency/article/001291.htm
- https://www.msdmanuals.com/professional/hematology-and-oncology/anemias-caused-by-hemolysis/overview-of-hemoglobinopathies
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163784/
- https://en.m.wikipedia.org/wiki/Hemoglobinopathy
- Source
- https://www.babysfirsttest.org/newborn-screening/conditions/hemoglobinopathies
- https://www.sciencedirect.com/topics/medicine-and-dentistry/hemoglobinopathy

Dear @jsalvage !
Daalụ for article!
I have no medical expertise, but I felt your intelligence was excellent!😃
Hello friend, thanks for stopping by today. What expertise do you have 😀
Translated as 이 기사에 감사드립니다.
i gisa-e gamsadeulibnida.
Dear @jsalvage !
James!
I have some knowledge about literature, art, history, and science.
How to interpret this sentence in English?
I just translated it for you in Korean 🤣...
In English, it means "Thank you for this article"
James! I understand!😃
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
You may also include @stemsocial as a beneficiary of the rewards of this post to get a stronger support.