Neuro Pathology || The Pathophysiology of Subdural Hematoma
Hey everyone, it is nice to be with you again today, and today as we continue our neuro pathology, I will be discussing Subdural Hematoma. As the name implies, it is bleeding that occurs in the subdural space. Before I continue, let me quickly do a quick anatomy of the subdural space.
Starting from the inner part of the skull is the bone of the skull which has underneath it the periosteal layer of the dura mater which is followed by the epidural space which separates the periosteal layer of the dura mater and the meningeal dura mater. below the meningeal dura mater is the arachnoid mater. Between the arachnoid mater and the Pia mater is the subdural space which we will be talking about. Below the Pia mater is the Brain parenchyma.

The subdural space is composed of veins known as the dural venous sinuses which include the superior sagittal sinuses and the inferior sagittal sinuses, and the bridging veins which collects blood from the cerebral cortex into the superior sagittal sinus. Subdural hematoma has to do with the rupturing, tearing, and perforation of the bridging veins basically a venous bleed of the bridging veins. Epidural hematomas are actually tearing in the arteries (the meningeal artery) but in sincerely rare cases there can be a venous epidural hematoma.
Subdural hematoma is usually caused by traumatic causes. Its etiology is usually as a result of trauma. This can lead to an acceleration-deceleration type of injury as a result of the brain smashing the skull forwards and backward stretching the bridging veins, causing them to tear during the process. Minor injuries in older persons can also lead to this bleeding as a result of cases such as cerebral atrophy where the brain size reduces as a result of old age and can also be a result of alcohol intake or neurodegenerative disease and minor falls can lead to the bleeding of the brain in the subdural space. Having thin Cerebral veins as in infants (Non Accidental Trauma) shaking baby syndrome and alcohol abuse can lead to the tearing of the bridging veins. ,
Normally, there are micro tears that form within blood vessels of the subdural space where platelets form a clot. In the case where a person has low platelet causing thrombocytopenia causing the inability of clotting on the vessels leading to bleeding in the area causing a subdural hematoma., Malignancy and tumors in the subdural space or Dural metastases cause blood to feed the growth and possibly lead to a tear of the vein causing a subdural hematoma., , Another cause would be intracranial hypertension as a result of a reduction of the cerebrospinal fluid in the epidural mater and dura mater causing the space to collapse and leading to a tear of the vein causing a subdural hematoma. This can be from a lumbar puncture. , ,
Subdural hematomas can be acute Subdural hematomas, subacute Subdural hematomas, and chronic Subdural hematomas. Acute Subdural hematomas have to do with blood which is fresh accumulating in the subdural space. In the case of sub-acute Subdural hematomas, the blood is starting to form a clot and exudated fluids are starting to form in the subdural space. People with sub-acute Subdural hematomas do not experience any symptoms until about 4 to 21 days. With Chronic Subdural hematomas, there is clotted blood already in the subdural space, and there is exudated fluid in the space already. This hematoma triggers the release of cytokines in the space causing the meningeal artery to allow neo capillaries to infiltrate the dura mater causing the leakage of fluids and inflammation., ,
Clinical features would include headache, loss of consciousness, and focal neuro deficits. Over time, as the bleeding increases, it can lead to subfalcine herniation where the brain tissue is pushed beneath the falx cerebri preventing blood to get to the cerebral cortex which can affect the cerebral motor cortex which controls the muscles of the lower extremities if the anterior cerebral artery isn't supplying it leading to weakness of the lower extremities and sensory loss. , If there is a bi-hemispheric subdural hematoma that compresses the brain tissue, this can compress the diencephalon from the subcortical region towards the brain stem downwards known as a diencephalic shift, and can lead to duress hemorrhages. With diencephalic shift, the sympathetic fibers are compressed leading to the inability to dilate the pupils. The diencephalon can also shift towards the dorsal midbrain causing upgaze palsy. If it affects the red nucleus, it would lead to an increase in the contraction of flexion muscles.,
It can also lead to uncal herniation where the uncus slips out of the tentorial cerebelli and then towards the midbrain causing an ipsilateral third nerve palsy leading to a down but outward movement of the eye, and a dilated pupil. The Uncus can also compress the cerebral peduncles damaging the corticospinal fibers and leading to contralateral and ipsilateral weakness of the muscles.,
High intracranial pressure as a result of the hematoma can lead to the compression of the optic nerve altering the venous drainage from the retina veins and leading to edema in the optic disc (papilledema), It can also lead to diplopia. High intracranial pressure can lead to a trigger of the chemo trigger zone leading to nausea and vomiting. Patients can also have herniation syndromes which would lead to infratentorial subdural hematomas where there is a bleed in the infratentorial area leading to a bleed in the brainstem, the cerebellum leading to brainstem compression, which can cause respiratory, and cardiovascular abnormalities. , ,
Image Reference
Image 1 || Wikimedia Commons || Types of Intracranial hematoma
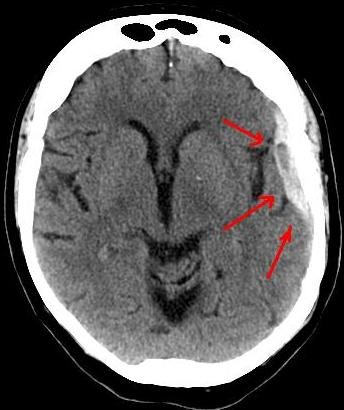
Image 2 || Wikimedia Commons || Ct-scan of the brain with an subdural hematoma
If this is not quickly treated, it can leads to death definitely
It is so funny how so many of us take some things with levity, such as shaking infants in the name of playing with them. I remember one time a woman was shaking a baby so hard in the name of playing with the baby. This baby wasn't even up to 6 months old. This issue of shaking babies is also common in Nigerian grandmothers and mothers who want to bathe infants. My grandmother would hold the baby by the legs and shake the baby and this is just similar to what other grandmothers do and when you ask them, they say it would make the baby strong. I guess most of us were just lucky not to have shaking baby syndrome which could lead to subdural hematoma.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.