Accuracy and Reliability of Thermometers: Assessing Body Temperature in Modern Healthcare
During the Covid-19 pandemic, there were a lot of thermometers flying around with one which became so popular in banks, and public places. We can testify that Covid-19 was a serious pandemic, and it thought us a lot of things but back to thermometers and body temperature.
Within the context of physical examination, body temperature is vital and that's why when a person tells you they have a headache, body pain, or any health concern that can be expressed physically the first thing that comes to mind is check if the temperature is still low. While checking temperature looks like a very simple endeavor, it isn't as simple as it looks and that is why there are equipment to check.
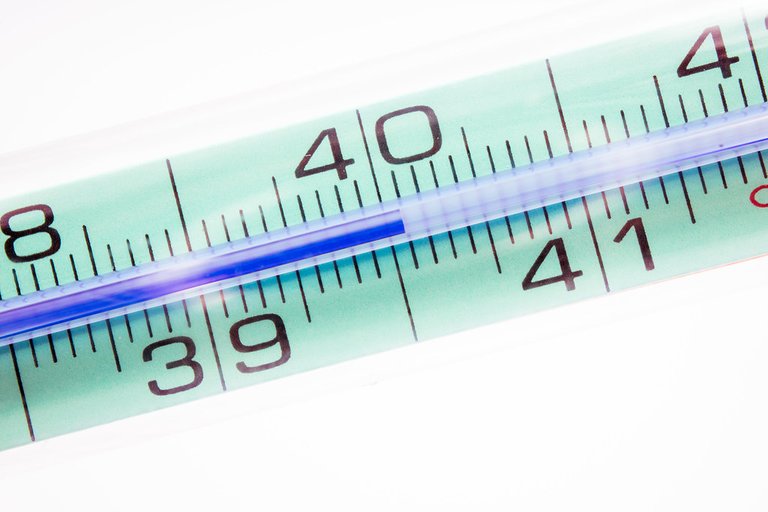
Image from Flickr
Except from critical care units that use more invasive methods of checking central temperature, there are four basic types or let me call it designs for peripheral temperature measurement in adults which check oral and axillary temperature, the ones that use infrared which are swept across the forehead or placed against the temporal artery, One placed inside the ear which measures tympanic temperature, and the one that you are very conversant with which is the non contact one. That one that you stand at its front and it just gives the body temperature from afar.
There have been reports and data reporting the accuracy of these thermometer, such as one titled "Accuracy of Peripheral Thermometers for Estimating Temperature" concluded that the Peripheral thermometers did not have clinically acceptable accuracy and further stated that it should not be used to determine clinical decisions when looking at body temperature. While another report titled "A systematic review of the accuracy of peripheral thermometry in estimating core temperatures among febrile critically ill patient" concluded that the thermometer that uses the tympanic and oral thermometry provided relatively accurate measures within the febrile range and could be used for the purpose.

Image From Pexels
With this reports, it then begs the question, should we be using peripheral temperature when checking the temperature of patients or do we use central temperature when checking temperature. Which of the temperature measurement correlates well with disease characterized by fever. While central temperature seems to be accurate at identifying fever pathologically, I didn't see much studies on this topic.
To assume that one type of thermometer is good or better, we need to first come to an understanding of what level does temperature amount to be fever. If you are asked the normal body temperature of a human, you would come to say 37oC or 98.6oF and it looks like this is changing. This standard temperature started in the 19th century when Carl Reinhold August Wunderlich studied temperature and he came with the mean temperature which we now take as standard, and he also made it known that fever was a symptom of a disease and not the disease itself, but things have changed over time. As at the time when he give the normal body temperature, there were a lot of diseases that we were still battling.

Image From easy-peasy.ai
If we are to look at the mean temperature of the time, we would see that it could be as a result of infection and disease prevalence around which increased body temperature, also the life expectancy at the time was 40 years. Research has been ongoing on the normal human body temperature and it from researches such as "Decreasing Human Body Temperature in the United States Since the Industrial Revolution" which shows convincing evidence that the average human body temperature is decreasing within the last 100 years as a result of decrease in disease prevalence.

Image FromPexels
According to some researches, like from the paper "Normal Oral, Rectal, Tympanic and Axillary Body Temperature Average in Adult Men and Women. A systemic Literature review" found 35.7-37.7oC and 33.2-38.1 oC, in rectal 36.7-37.5oC and 36.8-37.1oC, and in tympanic 35.5-37.5oC and 35.7-37.5oC in men and women respectively. Temperature is slightly higher in females than males and this temperature changes in women who are menstruating and ovulating. Also temperature changes depending on the time of the day, so using one temperature range as the normal temperature is completely flawed.
As our understanding of human physiology deepens, the methods for measuring body temperature and defining "normal" continue to evolve. While peripheral thermometers are convenient and widely used, their accuracy can vary. It's crucial to consider context and use the appropriate tool for the situation. As we move forward, ongoing research will help refine our approach to temperature measurement and the implications for medical care and public health.
Reference
https://www.sciencedirect.com/topics/nursing-and-health-professions/oral-thermometer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5012839/
https://www.acpjournals.org/doi/abs/10.7326/M15-1150?journalCode=aim
https://pubmed.ncbi.nlm.nih.gov/21880009/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8871951/
https://med.stanford.edu/content/dam/sm/epidemiology/documents/HRP236/Parsonnet---Critical-Appraisal-of-98.6F.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6946399/
https://pubmed.ncbi.nlm.nih.gov/12000664/
https://www.researchgate.net/publication/229738265_Normal_oral_rectal_tympanic_and_axillary_body_temperature_in_adult_men_and_women_A_systematic_literature_review
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.