A Critical Look at Antibiotic Resistance in Agriculture and Public Health
I saw an announcement by Chick-fil-A, making a commitment that by 2019, they were going to serve only chickens raised with no antibiotics. While the publication is quite old, it caught my attention. While it looked like the company was trying to market the making of natural food in their chain, it is no doubt that we need to start rearing antibiotics free chicken because there is a worry about antibiotic resistance especially from animal farming.
This is not the first time that public health organization has mentioned that bacteria are getting resistant to antibiotics and the result being the fact that agricultural animals are fed antibiotics even when they do not need them. The truth is, although we have enjoyed the importance of antibiotics for over 80 years, if we continue to use antibiotics the way we use them, something as little as a cut can cause us to lose our lives. This is very disturbing, but how did we get here?
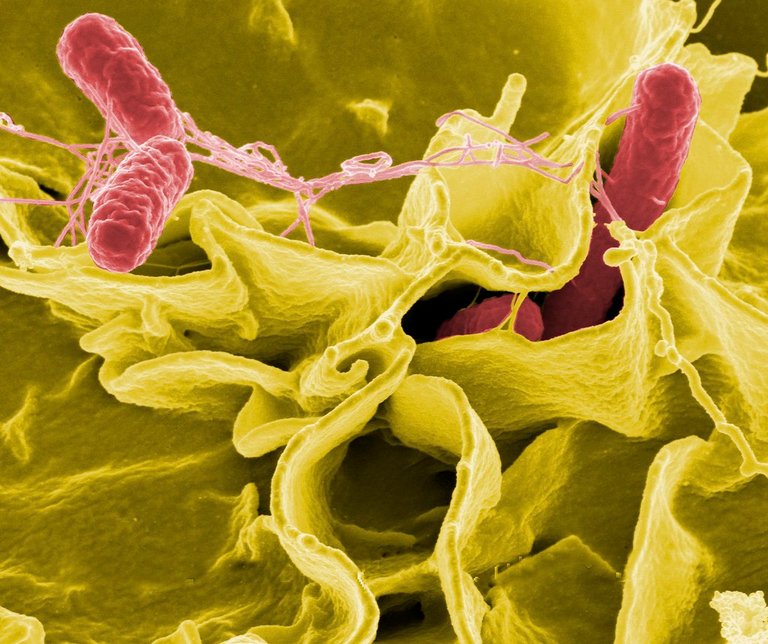
Antimicrobial resistance occur when pathogen (bacteria, virus, or fungi) no longer respond to medications that were initially designed to kill them. When pathogens become resistance, their infections can be hard to treat and fatal. Talking about bacteria, it is no doubt that when a high level of antimicrobial is added to germs that are susceptible to them, they kill them. But then some bacteria have certain resistance mechanisms that allows them to survive in the presence of this antibiotics. When the bacteria survive, they multiply to share the trait with their offsprings, creating a new strain of bacteria that share resistance mechanisms.
With bacteria, the use of selective pressure to survive in the midst of antibiotics is part of their lives. They can change their permeability limiting how the drug gets into the cells through the porins. This is common with gram negative bacteria that possesses cell membrane on both sides of their cell walls. Bacteria can also use Efflux pumps which are the little pores in the bacteria that helps to remove the antibiotics from the cell.
In other to resist drugs, the bacteria can modify the antibiotics target. For instance, penicillin binds to transpeptidase in bacteria but if the bacteria twerks the transpeptidase, then it will be difficult to the penicillin to bind with the transpeptidase. The final step is to use enzymes to destroy or change the antibiotics for instance, bacteria creating penicillinase will destroy penicillin.
That said, ho do bacteria begin to have these resistance? One is the intrinsic resistance (which is an innate trait in the bacteria that confers resistance to them and is independent of previous exposure to antibiotics). A very good example is using glycopeptides against gram-negative bacteria and the antibiotic not functioning because the the drug is enormous to cross the cell membrane. The second resistance is the acquired resistance and that is the scary one. Bacteria are able to replicate and mutate in the process thereby acquiring the mutated gene. These gene can be transferred to other bacteria in through conjugation, transduction, and Transformation.
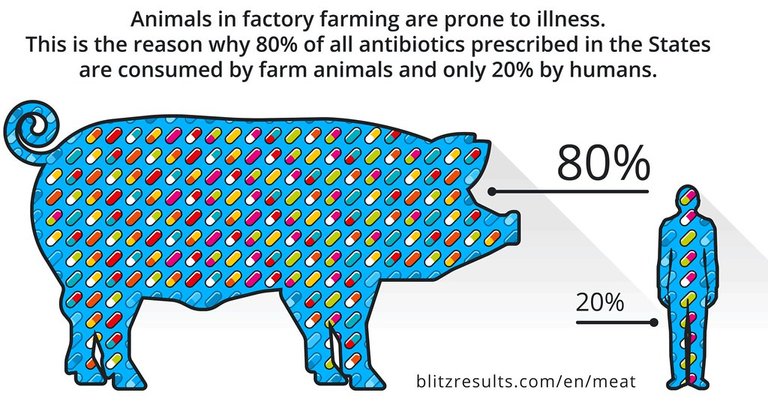
Bacteria Resistance has been caused by two parallel happenings which are both overuse. The Overuse of antibiotics in humans and in Agriculture. This Resistance didn't just start today, it has been since a very long time. Scientist like Alenxander Fleming talked about this resistance in his Nobel award in December 1945 where he mentioned the resistance to penicillin being caused by under dosing oneself with the drug not enough to cause death of the microbe thereby causing the microbe to be resistant.
In the 1980s, there was misuse of antibiotics, where doctors administered penicillin without knowing the cause of the disease, or when patients forced doctors to administer antibiotics to them when they did not need it. Also, certain companies added penicillin to everything. You might have thought that penicillin was the only drug but in reality it wasn't so because as new antibiotics that were promising were made, their usage cause for resistant bacteria which leads doctors to scientists to start looking for drugs that affects the new resistant strain of the bacteria. An example of such resistance is with the antibiotics Tetracyclines which was rolled out in the 1950s and by 1959 Tetracycline resistant Shigella was documented.
Soon bacteria began to become resistant to multiple drugs at the same time, and this happened because scientist decided to start using two types of drugs to attack bacteria that produced pennicilase but over time, there was a resistance to the drug. Bacteria began to grow resistance against combination antibiotics, and it was a problem but while we were looking to solve that, the agriculture world was doing something different.
In the 1940s, Thomas H. Jukes was looking for how animals would get vitamins B12 so as to make them healthy but wanted to get it in a cheap method. He also knew that the microbe that produced the antibiotics Stretomycin also produced B12 so they decided to do an experiment with chicks while giving them S. aureofaciens Mash (for Aureomycin) and they realized that the chicks lived, and they got bigger in respect to how much antibiotics they were fed.
Antibiotics soon became a problem when there was a staph outbreak across Blue Collar Men in Seattle in 1956, but the victims of this outbreak were not related, but they worked at the same poultry processing plant that Acronized meat (Deep the meat into antibiotics).
It is the 2000s and the antibiotics that used to be the miracle drugs are now looking like they aren't anymore. In 2016, a UN general Assembly of 70 government declared antibiotic resistance a global crisis, also WHO, FDA, G20, and G7 looked into antibiotics resistance. We are now looking for ways to solve this problems and according to the Guidance for Industry written by the FDA, asked pharmaceutical companies to remove growth promoting label from their antibiotic labeling. Farmers were also required to get a prescription from a veterinarian before using antibiotics for other purposes. These steps are to reduce the use of antibiotics in excess from farms.
Reference
https://pubmed.ncbi.nlm.nih.gov/35203785/
https://www.sciencedirect.com/science/article/pii/S1876034121003403#bib0115
https://www.nobelprize.org/uploads/2018/06/fleming-lecture.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4080027/
https://www.nature.com/articles/146837a0
https://www.sciencedirect.com/science/article/pii/S0021925818566837
https://journals.sagepub.com/doi/pdf/10.1177/003335491212700103
https://www.jstor.org/stable/4591310
https://www.cdc.gov/drugresistance/biggest-threats.html
https://www.nature.com/articles/s41599-018-0152-2
https://www.nature.com/articles/s41599-018-0181-x
https://www.cdc.gov/drugresistance/about.html
https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/antimicrobial-resistance-information-fda
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2937522/

Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.
The issue or talk about antibiotic resistance is something that we do not speak about loud enough, many people have had serious repercussions from its abuse and i am glad you took as through this, thanks for sharing